Every year, hundreds of thousands of older adults in the U.S. end up in the hospital because of a simple mistake: they took the wrong pill, at the wrong time, or too much of it. It’s not because they’re careless. It’s because managing multiple medications at home is confusing, overwhelming, and easy to mess up-especially when you’re dealing with memory lapses, poor eyesight, or just plain exhaustion. The good news? You don’t have to live with this risk. A medication safety at home system doesn’t need to be high-tech or expensive. It just needs to be smart, simple, and consistent.
Start with the List: Your Medication Bible
Before you buy a fancy dispenser or download an app, sit down with every pill bottle, supplement box, and prescription bag you have. Write down everything you take-name, dose, time of day, reason, and who prescribed it. Include over-the-counter drugs like ibuprofen, melatonin, or antacids. Don’t forget vitamins, herbal supplements, or patches. Many people forget these, but they’re just as likely to cause dangerous interactions as prescription meds. Use a printed sheet or a simple note app. Keep it updated. Every time your doctor adds, removes, or changes a medication, update the list immediately. Bring this list to every appointment-doctor, pharmacist, ER. It’s the single most effective thing you can do to prevent a medication error. The CDC says this step alone cuts error risk by nearly half.Match the Tool to Your Life
Not everyone needs a robot pill box. If you only take two pills a day, a basic AM/PM pill organizer costing $10 might be all you need. But if you’re juggling five or more medications, spread across four or more times a day, you need more than a plastic tray. Smart dispensers like Hero or MedMinder are designed for complex regimens. They hold up to 30 days of pills, dispense them automatically at set times, and send alerts to your phone and to a family member if you miss a dose. These devices aren’t magic-they require setup, but once configured, they work like clockwork. Studies show users stick to their schedules 98% of the time with these systems, compared to under 70% without. Here’s what to consider when choosing:- Basic organizer ($5-$25): Good for simple routines. No reminders. No tracking. Only use if you’re sharp, organized, and take few meds.
- Smart dispenser ($150-$300 + $15-$50/month): Best for people on 5+ daily doses. Alerts, remote monitoring, and dose history. Requires Wi-Fi and smartphone.
- Digital platform like HomeMeds (free app or clinic-assisted): Lets you scan pill labels with your phone to auto-fill your list. Great for caregivers helping from afar. New AI version launching Fall 2025 will cut assessment time in half.
Setup Isn’t a One-Time Task
Buying a smart dispenser doesn’t mean you’re done. Setup takes 2-4 hours. You need to:- Sort every pill into the correct compartment by time and day.
- Program the device with exact times (e.g., 7 a.m. with breakfast, 7 p.m. with dinner).
- Connect it to Wi-Fi and your phone.
- Teach a family member how to check the app for missed doses.
- Test it with a dummy day-set it to remind you to take a candy or a bottle of water at 3 p.m. to make sure the alarm works.

Handle the Messy Stuff
Not all meds fit neatly into a dispenser. As-needed pills-like painkillers, nitroglycerin, or anti-anxiety meds-can’t be pre-loaded. Same goes for insulin, inhalers, or eye drops. These need their own system. Use a small, labeled container or a sticky note on the fridge. For example: “Take 1 tablet for chest pain-call 911 if no relief in 5 min.” Put it where you’ll see it. If you use a rescue inhaler, keep it next to your toothbrush or coffee maker-places you go daily. Also watch out for special instructions: “Take on empty stomach,” “Avoid grapefruit,” “Take with food.” Write these on the pill bottle or next to the dispenser. Many errors happen because people don’t know how to take the pill, not that they forget it.Keep the System Alive
Medication changes happen. A new diagnosis. A side effect. A cheaper generic. Each change breaks your system if you don’t update it. Set a monthly “med check” with your caregiver or yourself. Look at your list. Compare it to your bottles. Ask: Did my doctor change anything? Did I skip a dose? Did the pharmacy give me a different-looking pill? If you use a smart dispenser, call the company if you need to swap a pill. Most won’t let you reprogram it yourself-too risky. They’ll send a technician or guide you over the phone. Don’t try to force a pill into the wrong slot. That’s how errors start.Who’s Watching?
No system works if no one’s checking in. Even the best dispenser can’t tell if you’re feeling dizzy, nauseous, or confused after taking a new med. That’s where human backup comes in. Designate one person-a spouse, child, neighbor, or home health aide-to get weekly alerts from your device. Make sure they know how to respond: “If Mom misses two doses in a row, call the pharmacist.” Studies show that when caregivers are involved, adherence jumps from 85% to 98%. That’s the difference between staying out of the hospital and ending up there.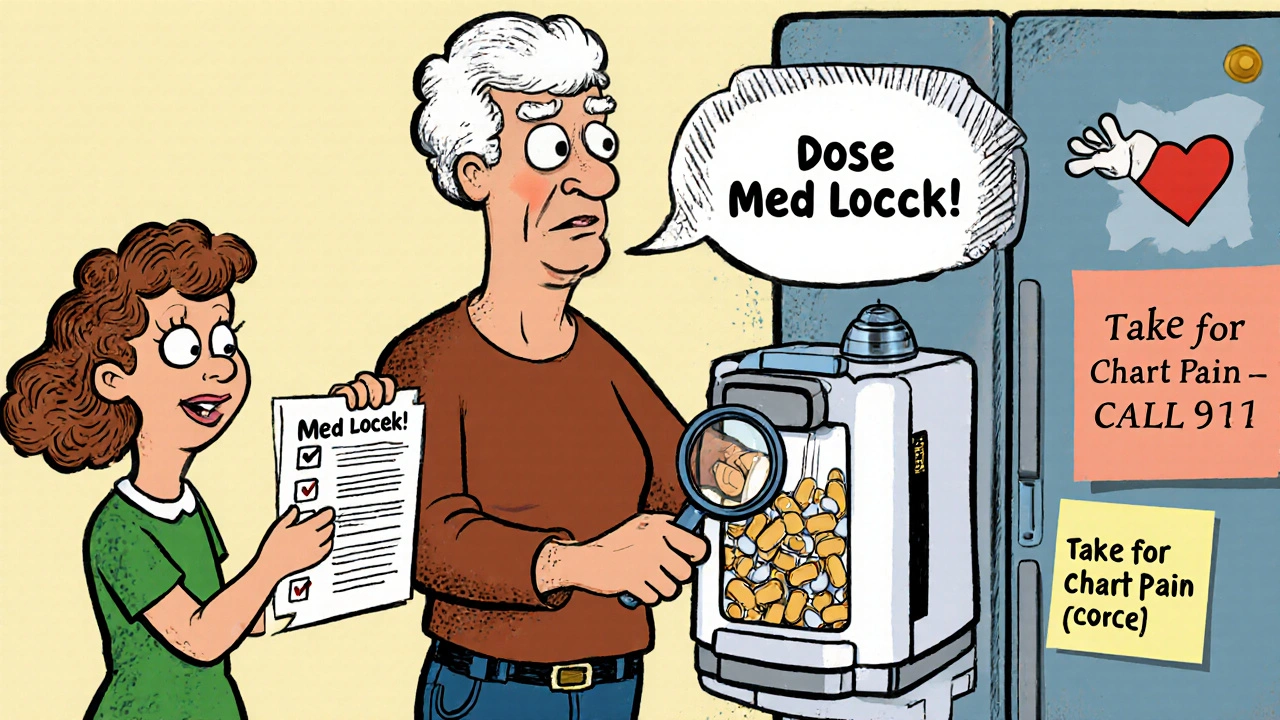
What to Avoid
Here are the top three mistakes people make:- Using old pill bottles. If you refill a bottle but don’t update the label, you’re playing Russian roulette with your meds.
- Sharing meds. Your arthritis pill is not your husband’s. Ever. Even if the pills look alike.
- Ignoring side effects. Dizziness? Fatigue? Confusion? Don’t brush it off as “getting older.” It could be a drug interaction. Call your doctor or pharmacist immediately.
What’s Coming Next
The field is moving fast. By 2027, most smart dispensers will check for dangerous drug interactions automatically. Some will use voice commands for people with poor vision. Others will sync with your electronic health record so your doctor sees your real-time adherence. The biggest breakthrough? AI-powered platforms like HomeMeds’ new version, launching Fall 2025. It’ll scan your pill bottle with your phone camera and auto-fill your list. No typing. No guessing. Just point, snap, and done. But tech won’t fix everything. As Dr. Sarah Chen, a geriatric pharmacist, says: “Tools help. But education and regular reviews save lives.”Start Small. Stay Consistent.
You don’t need to overhaul your whole system tomorrow. Pick one thing: make your medication list today. Put it on the fridge. Update it after your next doctor visit. That’s it. That’s the foundation. From there, add one layer at a time. A pill organizer next week. A family alert the week after. A smart dispenser when you’re ready. Medication safety isn’t about perfection. It’s about reducing risk. One less mistake. One fewer hospital trip. One more day you feel like yourself.What’s the most common cause of medication errors at home?
The most common cause is a mismatch between what’s on the patient’s list and what’s actually being taken. This happens when people stop or start meds without updating their list, refill prescriptions with different-looking pills, or forget to include over-the-counter drugs and supplements. The CDC says keeping an accurate, real-time list reduces errors by up to 48%.
Are smart pill dispensers worth the cost?
For people taking five or more medications daily, yes. The upfront cost ($150-$300) plus monthly fees ($15-$50) may seem high, but consider this: one preventable hospital admission due to a medication error can cost $15,000-$30,000. Studies show smart dispensers reduce missed doses by over 90%, which cuts ER visits and readmissions. Many Medicare Advantage plans now cover part or all of the cost-check with your provider.
Can I use a regular pill organizer if I have memory issues?
Not reliably. A basic AM/PM organizer only holds pills-it doesn’t remind you to take them. If you forget to check the box, you’ll miss doses. For memory issues, you need alerts: phone notifications, voice prompts, or caregiver notifications. A smart dispenser or digital app with reminders is far safer.
What if I can’t afford a smart dispenser?
Start with free or low-cost options. Use a printed medication list. Set phone alarms labeled with each med’s name and time. Ask your pharmacist for a blister pack-some pharmacies offer free pre-sorted weekly packs. Contact local Area Agencies on Aging-they often have programs that lend dispensers or offer financial help. The National Council on Aging says 22% of low-income seniors can’t afford tech, but many community resources exist.
How often should I review my meds?
Every 30 to 90 days. Even if nothing changed, review your list, bottles, and dispenser. Look for expired meds, duplicate prescriptions, or pills that look different. Schedule a “brown bag” review with your pharmacist once a year-bring everything you take, and they’ll check for interactions, redundancies, and unnecessary drugs. Many pharmacists do this for free.
Do I need Wi-Fi for a smart dispenser?
Most do. Wi-Fi lets the device send alerts to your phone and caregivers, and syncs data to the cloud. If you don’t have reliable internet, look for models with cellular backup or offline modes. Some dispensers store data locally and sync later. Ask the company before buying. If you’re in a rural area with poor signal, a basic organizer with alarms on your phone might be a better fit.
Can I use these systems if I have poor vision or arthritis?
Yes, but choose wisely. Look for dispensers with large buttons, voice prompts, or smartphone apps with text-to-speech. Some models now support voice commands-just say, “Take my morning pill,” and it opens. For arthritis, avoid devices with small compartments or tricky lids. Ask your pharmacist for models designed for low dexterity. The NIH is funding voice-activated dispensers for visually impaired users, launching in 2026.
What should I do if I miss a dose?
Don’t double up unless your doctor says so. Check the label or call your pharmacist. Many meds are safe to take late; others aren’t. If you miss a dose and feel unwell-dizzy, nauseous, or confused-call your doctor immediately. If you use a smart dispenser, the alert will notify your caregiver, who can help you decide what to do next. Never guess.
Vera Wayne
I started using a printed med list after my mom nearly took two blood pressure pills by accident. Now I update it after every doctor visit-handwritten, in pen, and taped to the fridge. It’s low-tech, but it works. I also have my daughter check it every Sunday. Simple? Yes. Life-saving? Absolutely.
Rodney Keats
Wow. A 300-dollar robot that tells you when to take your pills. Next they’ll sell us a teddy bear that whispers, ‘Don’t forget your aspirin, sweetie.’
Laura-Jade Vaughan
OMG YES 💯 I just got my Hero dispenser last month and it’s a GAME CHANGER. 🤖✨ My grandma used to hide her pills in the cookie jar-now she gets a voice alert and a text to my phone. Also, the app has a little ‘Good job!’ animation when she takes her meds. I cried. This is what aging with dignity looks like. 🥹❤️
Jennifer Stephenson
Make a list. Update it. Use alarms. That’s all you need.
Segun Kareem
In my village in Nigeria, we don’t have smart dispensers. But we have something better: community. When someone’s sick, the whole block knows their meds. Someone brings the pills. Someone reminds them. No Wi-Fi needed. Tech is great-but human connection? That’s the real safety net.
Sharon Campbell
you know what’s really dangerous? trusting big pharma’s ‘solutions’. those smart dispensers? they’re just tracking your data for insurance companies. next thing you know, they’ll raise your rates if you ‘miss’ a dose. also, who says you need to take all these pills anyway? i stopped mine and now i feel way better. lol
sara styles
Let me guess-this whole article was written by a pharmaceutical rep with a marketing budget. Smart dispensers? They’re designed to keep you dependent on pills, not cure anything. The CDC? They’re funded by Big Pharma. Did you know the FDA approved 89% of drugs based on industry-funded studies? And don’t get me started on how they suppress natural alternatives. Your ‘med list’? That’s just the first step to being fully monitored. Your phone, your dispenser, your doctor-they’re all connected. You’re being tracked. And you’re okay with that? Wake up.
Brendan Peterson
The article’s solid, but it underestimates the burden of setup. If you’re 82 with arthritis and no tech skills, ‘teach a grandkid’ is unrealistic. Most grandkids are busy or live across the country. The real gap isn’t tech-it’s access to hands-on help. Pharmacies should offer free in-home setup. Period.
Jessica M
As a geriatric pharmacist with over 20 years of experience, I can confirm: the most effective intervention remains the accurate, up-to-date medication list. I have seen patients avoid hospitalization repeatedly simply because they brought their list to the ER. No device replaces human verification. I recommend printing two copies-one for the patient, one for the caregiver-and reviewing them together monthly. This is not optional-it is standard of care.
Erika Lukacs
One wonders whether the true purpose of these systems is safety-or the normalization of surveillance in the private sphere. Is our autonomy being quietly exchanged for the illusion of security?
Rebekah Kryger
Let’s be real-most of these ‘smart’ systems are just glorified timers with subscription traps. The real solution? Deprescribing. Reducing polypharmacy. But nobody wants to talk about that because it doesn’t sell gadgets. Also, ‘blister packs’ are cheaper, FDA-regulated, and don’t require Wi-Fi. Why isn’t that the first recommendation?
Victoria Short
eh i just use my phone alarms labeled ‘blue pill’ and ‘white pill’ and it’s fine. no need to overcomplicate it.