Meglitinide Hypoglycemia Risk Calculator
Enter the time you take your meglitinide medication and when you plan to eat to calculate your hypoglycemia risk level.
When you’re managing type 2 diabetes, meal timing isn’t just about nutrition-it’s a matter of safety. For people taking meglitinides, skipping a meal can send blood sugar crashing faster than most other diabetes drugs. Unlike long-acting pills that work all day, meglitinides act like a quick flash: they trigger insulin release within minutes, and if food doesn’t follow, your blood sugar drops dangerously low. This isn’t a theoretical risk. It’s a real, documented danger tied directly to how these drugs work.
How Meglitinides Work (and Why Timing Matters)
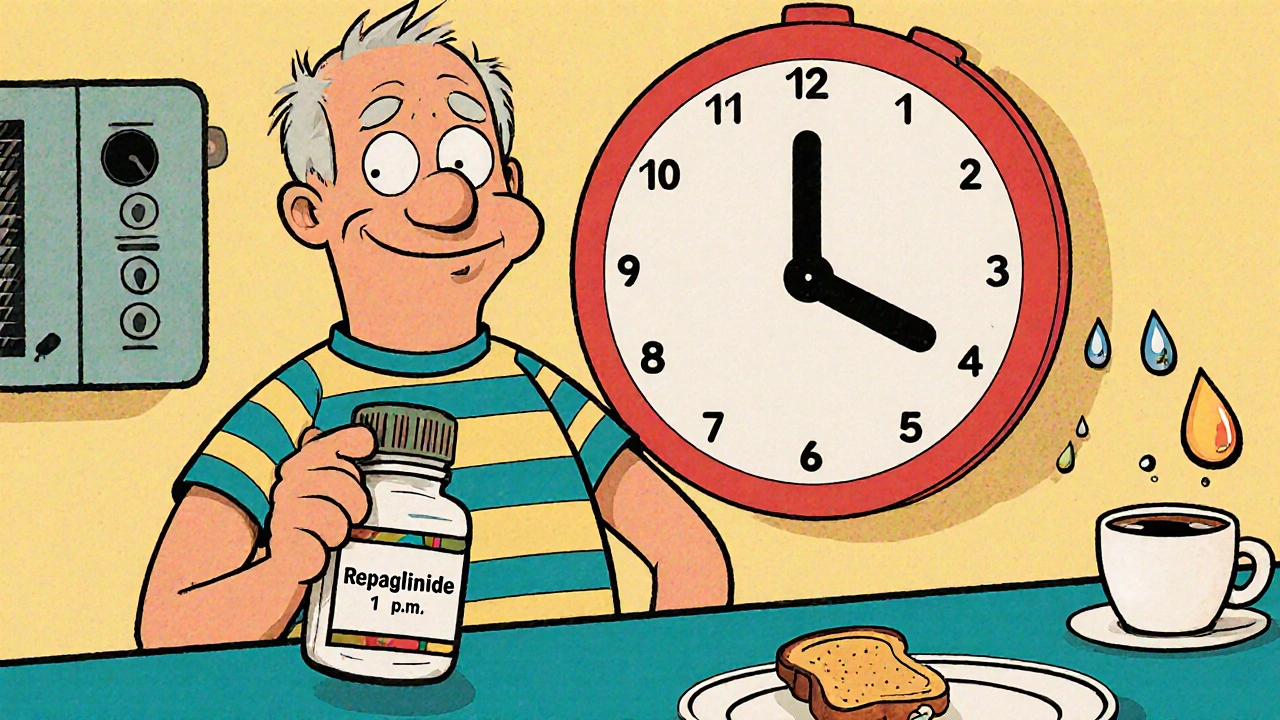
Meglitinides-mainly repaglinide and nateglinide-are fast-acting drugs designed for people who don’t eat at the same time every day. They bind to receptors on pancreatic beta cells, forcing them to release insulin right away. Repaglinide starts working in 3 to 5 minutes; nateglinide kicks in even faster, within 1 minute. Both peak in about an hour and are mostly gone from your system in 2 to 4 hours.
This speed is the whole point. If you’re eating lunch at 1 p.m. one day and 7 p.m. the next, you don’t want a drug that’s still pumping out insulin at midnight. Meglitinides were made for that flexibility. But here’s the catch: they only work if you eat. No meal? No insulin signal. But the insulin is already there, circulating in your blood. That’s when your glucose levels start falling.
Clinical studies show that skipping just one meal after taking a meglitinide increases your risk of hypoglycemia by 3.7 times. Blood sugar can dip below 70 mg/dL within 90 minutes. That’s not just feeling shaky-it’s confusion, sweating, dizziness, and in severe cases, seizures or loss of consciousness.
Who’s at Highest Risk?
Not everyone on meglitinides will have problems. But certain groups face much higher danger.
- Older adults: Cognitive decline, memory issues, or simply forgetting meals can turn this drug into a hazard. The American Diabetes Association’s 2025 guidelines specifically warn that irregular eating patterns are a major reason older patients on these drugs end up in the ER.
- People with kidney disease: While repaglinide is cleared by the liver (making it safer than sulfonylureas in kidney patients), those with advanced chronic kidney disease (eGFR below 30) still face a 2.4-fold higher risk of hypoglycemia. Dosing must be cut in half-60 mg instead of 120 mg-according to kidney health guidelines.
- Those on multiple diabetes drugs: Combining meglitinides with insulin or sulfonylureas multiplies the risk. One study found that using meglitinides with insulin raised hypoglycemia rates significantly (p=0.018). The combined insulin surge can overwhelm your body’s ability to compensate.
Even healthy people aren’t immune. A 2023 study tracking real-world use found that 41% of all hypoglycemia events in meglitinide users happened 2 to 4 hours after dosing-the exact window when the drug is peaking and meals are often delayed.
How Meglitinides Compare to Other Diabetes Drugs
It helps to understand where meglitinides fit among other oral diabetes medications.
| Drug Class | Duration of Action | Hypoglycemia Risk | Meal Timing Flexibility |
|---|---|---|---|
| Meglitinides (repaglinide, nateglinide) | 2-4 hours | High if meals skipped | High-dose only when eating |
| Sulfonylureas (glipizide, glyburide) | 12-24 hours | High-always | Low-must eat regularly |
| Metformin | 6-8 hours | Very low | None needed |
| GLP-1 agonists (semaglutide) | 24+ hours | Low unless combined with insulin | High |
Sulfonylureas are the biggest contrast. They force insulin out all day, no matter if you eat or not. That’s why they cause hypoglycemia even during sleep or between meals. Meglitinides are more targeted-but only if you use them correctly. If you take repaglinide at 8 a.m. because you think you’ll eat soon, and then your day gets chaotic and lunch turns into dinner, you’re setting yourself up for a crash.

What to Do: Practical Rules for Safe Use
If you’re prescribed a meglitinide, your safety depends on three things: timing, consistency, and awareness.
- Dose only when you’re about to eat. Take it 15 minutes before your meal-not before you leave the house, not before your morning coffee, not because it’s “time.” If you’re unsure you’ll eat, skip the dose.
- Never skip meals after taking it. Even a light snack counts. A small apple, a handful of nuts, or a slice of toast can prevent a dangerous drop. Don’t wait for a “full meal.”
- Know the signs of low blood sugar. Shaking, sweating, hunger, dizziness, confusion, rapid heartbeat. If you feel any of these, check your glucose. If it’s below 70 mg/dL, take 15 grams of fast-acting sugar-glucose tablets, juice, or candy-and recheck in 15 minutes.
- Use reminders or apps. A 2023 trial showed that smartphone alerts reminding patients to eat after dosing cut hypoglycemia events by 39%. Set a phone alarm for 15 minutes after you take your pill. If you don’t eat by then, call someone or take a snack.
- Consider continuous glucose monitoring (CGM). If your meals are unpredictable, a CGM can alert you to drops before you feel them. Studies show CGM reduces hypoglycemia episodes by 57% in meglitinide users with irregular schedules.
Some patients are told to take meglitinides “with meals,” but that’s too vague. The real rule is: take it right before you start eating, and only if you’re going to eat. This is called the “dose-to-eat” approach-and it’s the gold standard for safety.
Why Are These Drugs Still Used?
You might wonder: if the risk is so high, why do doctors still prescribe them?
Because for some people, they’re the best option.
They’re often used when metformin doesn’t control post-meal spikes, or when sulfonylureas cause too many low blood sugar episodes. They’re also preferred in patients with kidney problems because repaglinide is cleared by the liver, not the kidneys. Around 4.2% of U.S. adults with type 2 diabetes are on meglitinides-small, but meaningful.
They’re especially helpful for shift workers, people with irregular work hours, or those with dementia or mental health conditions that disrupt eating patterns. For these individuals, a drug that doesn’t linger is better than one that does.
Still, the market is shifting. Newer drugs like GLP-1 agonists (semaglutide, liraglutide) are becoming first-line because they lower blood sugar without causing hypoglycemia-unless paired with insulin or meglitinides. But they’re expensive, and not everyone can use them.

The Future: Better Tools, Safer Use
Researchers are working on solutions. One promising development is an extended-release version of repaglinide (repaglinide XR). Early trials show it reduces hypoglycemia by 28% in people with unpredictable meals-without losing the meal-time flexibility. Phase II results are encouraging, and if approved, it could change how we use these drugs.
Also, integrated digital tools are becoming part of care. Apps that sync with glucose monitors, send meal reminders, and alert caregivers when blood sugar drops are now being tested in clinics. The goal isn’t to replace patient responsibility-it’s to support it.
But no tech can replace education. The FDA added stronger warnings to meglitinide labels in 2021, requiring explicit language about hypoglycemia risk when meals are skipped. That’s a good start. But real safety comes from understanding: this drug doesn’t work unless you do.
Final Takeaway
Meglitinides aren’t dangerous drugs. They’re powerful tools-with strict rules. Their biggest flaw isn’t the science. It’s the assumption that flexibility means freedom. It doesn’t. It means responsibility.
If you’re on repaglinide or nateglinide, your meals aren’t optional. They’re part of your medication schedule. Skip one, and you risk a medical emergency. Eat regularly, even if it’s small. Use reminders. Monitor your levels. Talk to your doctor if your schedule changes.
These drugs help people live better. But only if you treat them with the care they demand.
Jacob McConaghy
I’ve been on repaglinide for two years now, and honestly, I thought I was fine skipping meals if I was busy. Until I passed out in the grocery store last winter. Turned out my blood sugar was 48. Never again. Now I keep granola bars in every bag, car, and drawer. Even if I’m not hungry, I eat something. This drug doesn’t play around.
Also, the CGM tip? Life-changing. I got one last month and it saved me twice already. No more guessing when I feel weird. Just check my phone and boom-time to eat.
Natashia Luu
It is deeply concerning that physicians continue to prescribe medications with such a high potential for life-threatening adverse events without implementing mandatory patient education protocols. The current paradigm of patient responsibility is archaic and negligent. One cannot reasonably expect individuals with cognitive decline, erratic work schedules, or mental health comorbidities to maintain perfect temporal adherence to pharmacological regimens. This is not patient error-it is systemic failure.
akhilesh jha
Interesting. In India, we don’t have many people on meglitinides because they’re expensive and not covered by insurance. Most use metformin or gliclazide. But I’ve seen elderly patients skip meals because they forget or don’t feel like eating-then end up in the hospital with low sugar. No one tells them about the timing. Even doctors sometimes say ‘take with food’ and leave it at that.
Maybe the real issue isn’t the drug-it’s how we communicate. People need simple, visual reminders. Like a sticker on the pill bottle: ‘No eat? No pill.’
Jeff Hicken
so like… if i take my pill and then get stuck in a meeting and dont eat till 8pm… im basically a walking zombie? lol. jk but also not. i did that last week and my hands were shaking like i had caffeine overdose. turned out i was at 59. i ate a whole bag of gummies and felt like a new person.
why dont they just make these drugs slower? like… why the rush? also why is this not on the box like a warning label with a skull??
Vineeta Puri
Thank you for this comprehensive and clinically accurate overview. The emphasis on the ‘dose-to-eat’ principle is essential and often overlooked in primary care settings. I have observed in my practice that patients frequently misunderstand the phrase ‘take with meals’ as synonymous with ‘take during the day.’ Clarifying that the medication must be administered immediately prior to ingestion, and only if consumption is certain, is critical for safety.
I strongly recommend that healthcare providers use the ‘teach-back’ method when prescribing meglitinides: ask the patient to explain in their own words when and why they should take the medication. This reduces errors by over 60% in longitudinal studies.
Andy Louis-Charles
Just got my CGM last week and it’s been a game-changer. I’m on repaglinide and work nights, so meals are all over the place. Before, I’d get shaky at 3 a.m. and think it was just stress. Turns out, I was crashing hard. Now my phone buzzes at 68 and I grab a banana. No drama.
Also, the 15-minute rule? I set a reminder called ‘EAT OR SKIP’ that pops up after I take my pill. If I don’t tap ‘ate,’ it texts my wife. She’s my personal hypoglycemia watchdog. 😅
Douglas cardoza
bro i took my pill at 10am because i was gonna eat lunch, then got caught up in a call and didn’t eat till 5pm. felt like death. had to chug a juice box in the parking lot. this shit is wild. why do they even make it like this? why not just give us metformin and be done? i’m just trying to survive my day, not be a pharmacist.
Adam Hainsfurther
I’m a shift worker on the night crew, and meglitinides were the only thing that didn’t make me crash after eating at 3 a.m. Sulfonylureas made me hypoglycemic at 2 a.m. even if I hadn’t eaten. But this? It’s perfect if you’re disciplined.
My trick: I always eat a protein bar right after my pill. Doesn’t matter if I’m tired or not. I treat it like brushing my teeth. No exceptions. I’ve been on it for 3 years and never had a bad episode. It’s not the drug’s fault-it’s the mindset. You gotta treat it like a ritual.
Rachael Gallagher
Americans are too lazy to eat on time. That’s the real problem.