When you take a pill, you might assume it works the same way no matter what it’s called. But extended-release and immediate-release medications aren’t just different names-they’re completely different systems with different risks, timing, and real-world consequences. Getting this wrong can mean the difference between stable control of your condition and a dangerous overdose.
How Extended-Release and Immediate-Release Work
| Feature | Immediate-Release (IR) | Extended-Release (ER) |
|---|---|---|
| Time to peak effect | 30-90 minutes | 2-4 hours |
| Duration of effect | 4-8 hours | 12-24 hours |
| Dosing frequency | 2-4 times daily | 1-2 times daily |
| Peak-to-trough ratio | 3:1 or higher | 1.5:1 or lower |
| Absorption time | 4-6 hours | 12-24 hours |
Immediate-release pills dissolve fast. You swallow them, and within an hour, your bloodstream gets a full blast of the drug. That’s great if you need quick relief-like a painkiller for a sudden headache or an ADHD med before a big meeting. But it also means your drug levels spike high, then crash. That rollercoaster can cause side effects: jitteriness, nausea, or even seizures in high-risk cases.
Extended-release pills are built to move slowly. They use special coatings, tiny pellets, or osmotic pumps to let the drug leak out over many hours. Think of it like a slow drip instead of a firehose. For drugs like bupropion (for depression or smoking cessation), the IR version can spike blood levels above 400 ng/mL in two hours-dangerously close to the 350 ng/mL seizure threshold. The ER version keeps levels steady between 100-200 ng/mL all day. No spikes. No crashes.
Why Timing Matters More Than You Think
People often think, “If I don’t feel it right away, it’s not working.” That’s a dangerous assumption with ER meds. If you take your extended-release metoprolol for high blood pressure and don’t feel dizzy or lightheaded within an hour, you might be tempted to take another pill. But ER metoprolol takes 2-4 hours just to start working. By the time you take a second dose, you’ve doubled your intake-and you’re still waiting for the first one to kick in. That’s how accidental overdoses happen.
Studies show 41% of patients on ER medications initially struggle with this delay. About 28% end up taking extra doses because they don’t feel immediate effects. That leads to 9% reporting adverse events like dizziness, low heart rate, or confusion. The FDA has issued warnings about this exact pattern with extended-release opioids, antidepressants, and blood pressure meds.
On the flip side, IR versions are lifesavers in emergencies. If you’re having a panic attack and your ER sertraline hasn’t built up yet, you can’t rely on it for instant relief. That’s why many psychiatrists prescribe both: ER for daily stability, IR for breakthrough symptoms. Same drug, two different tools.
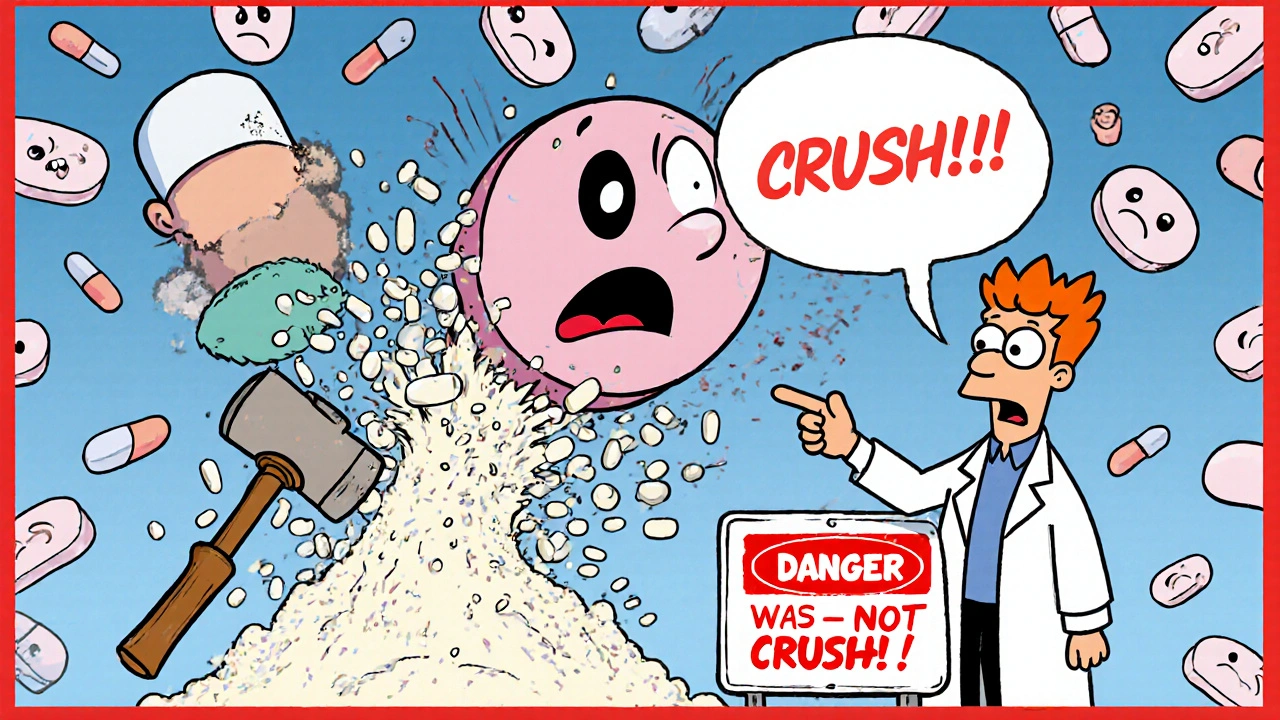
The Hidden Risks of Crushing, Splitting, or Chewing
It’s not just about timing-it’s about structure. Over 92% of extended-release tablets are not meant to be broken, crushed, or chewed. That’s not a suggestion. It’s a safety rule backed by the FDA.
Take Concerta, a popular ADHD medication. It uses an osmotic pump: a tiny tablet inside a shell that slowly pushes the drug out through a laser-drilled hole. If you crush it, you’re opening a floodgate. You get the full 36mg dose all at once. That’s not just ineffective-it’s dangerous. The same goes for OxyContin, Venlafaxine XR, and many others.
Pharmacists report that 23% of medication errors involving ER drugs come from patients splitting pills. Some tablets have a score line, but that doesn’t mean it’s safe. Venlafaxine XR, for example, has a score but still contains a complex matrix that can’t be evenly divided. Crushing it destroys the time-release mechanism. The result? A sudden, toxic spike in drug levels.
Always check the label. If it says “do not crush or chew,” that’s not fine print. It’s your warning sign.
When to Choose ER Over IR-and When Not To
For chronic conditions, ER is usually the better choice. A 2022 study of 15,000 hypertension patients found that 78% of those on ER medications stayed adherent over a year, compared to just 56% on IR. Why? Fewer pills. Less hassle. Fewer missed doses. That’s huge for conditions like diabetes, high blood pressure, or depression, where consistency matters more than speed.
The American Psychiatric Association recommends ER formulations for long-term mental health treatment because stable blood levels reduce side effects like insomnia or mood swings. For example, quetiapine XR causes fewer sleep disruptions than the IR version because it doesn’t create the sharp highs and lows that disrupt circadian rhythms.
But ER isn’t always right. If you’re starting a new medication, your doctor needs to fine-tune the dose. That’s where IR shines. You can adjust by 5mg or 10mg increments without waiting days for the full effect. Same with acute situations: a sudden flare-up of pain, a panic attack, or a seizure risk. IR gives you control. ER doesn’t.
And don’t forget the cost. ER versions often cost 15-25% more. Adderall XR might run $350-$450 for 30 capsules, while IR is $280-$380. That’s not trivial. If you’re on a tight budget and your condition is stable, IR with a strict schedule might be safer and cheaper than ER with a risk of accidental overdose.
Special Cases: Who Needs Extra Caution
Some people are at higher risk with ER meds-and they might not even know it.
If you have gastroparesis (delayed stomach emptying), your body holds onto ER pills longer than normal. That can cause drug levels to spike 30-50% higher than expected. The FDA issued a warning about this in July 2023, specifically calling out ER medications for diabetes, depression, and Parkinson’s.
Older adults often have slower digestion, kidney function, or liver metabolism. That means ER drugs can build up in their systems faster than intended. A once-daily dose might become a two-day dose. That’s why geriatric prescriptions often start lower and increase slowly.
And if you’re taking multiple medications, ER formulations can interact in unpredictable ways. A slow-release blood thinner combined with an ER painkiller? That’s a recipe for internal bleeding if the timing gets off.

What to Do If You’re on ER Medication
- Take it at the same time every day. Don’t skip doses or double up.
- Never crush, split, or chew unless your pharmacist or doctor explicitly says it’s safe.
- Wait at least 2-4 hours before assuming it’s not working. Don’t take more.
- If you miss a dose, don’t double up the next day. Call your provider.
- Keep IR versions on hand only if prescribed for breakthrough symptoms.
- Use a pill organizer with time labels-not just morning and night, but “ER AM” and “IR PRN.”
One patient on Reddit summed it up: “I use Adderall XR for work because it’s smooth all day. But I keep 5mg IR tabs for presentations. If I need focus right now, I need it right now.” That’s smart. It’s not about which is better-it’s about which is right for the moment.
What’s Changing in 2025
New technologies are making ER drugs smarter. Some ADHD meds now have “abuse-deterrent” coatings that turn into a thick gel when crushed-making them harder to snort or inject. In 2023, these reduced abuse potential by 47%.
And in labs, researchers are testing 3D-printed “polypills” that release different drugs at exact times. One pill could give you a blood pressure med at 7 a.m., a cholesterol drug at noon, and a sleep aid at 10 p.m. It’s still in trials, but it shows where the future is headed: personalized timing, not one-size-fits-all.
But until then, the rules are simple: Know your pill. Know your timing. Know your risk.
Can I split my extended-release pill if it has a score line?
No-not unless your doctor or pharmacist specifically says it’s safe. Even if a tablet has a score line, the coating or matrix inside may not split evenly. Crushing or splitting can release the full dose at once, leading to overdose. Always check the FDA-approved labeling or ask your pharmacist before altering any ER medication.
Why does my ER medication take so long to work?
Extended-release formulations are designed to release medication slowly over 12-24 hours. It can take 2-4 hours just to reach therapeutic levels, and up to 7-10 days to reach steady state in your body. If you expect instant results like with immediate-release pills, you might take extra doses-dangerously increasing your risk of overdose. Patience is part of the treatment.
Is extended-release always better than immediate-release?
No. ER is better for long-term stability and adherence, but IR is essential for titration (dose adjustment), acute symptoms, and emergencies. For example, someone with depression might take an ER antidepressant daily but keep an IR version for panic attacks. The choice depends on your condition, lifestyle, and how your body responds.
Can I take ER and IR versions of the same drug together?
Yes-but only under medical supervision. Some patients are prescribed both: ER for baseline control and IR for breakthrough symptoms. But combining them without guidance can lead to dangerous drug levels. Never mix them unless your prescriber has mapped out the exact timing and dosage.
What should I do if I accidentally crush or chew an extended-release pill?
Call your doctor or poison control immediately. You may have taken a full dose all at once. Symptoms of overdose vary by drug but can include rapid heartbeat, confusion, seizures, or extreme drowsiness. Do not wait for symptoms to appear. Time matters-especially with ER drugs that keep releasing into your system for hours.
Are extended-release medications more expensive?
Yes, typically by 15-25%. For example, Adderall XR costs about $350-$450 for 30 capsules, while Adderall IR is $280-$380 for the same total daily dose. But ER often improves adherence, which can reduce long-term healthcare costs from missed doses or complications. Check your insurance coverage-some plans cover ER versions with lower copays to encourage better outcomes.
Can I switch from IR to ER without consulting my doctor?
Never. Switching between IR and ER isn’t just a dosage change-it’s a pharmacokinetic change. The same milligram amount doesn’t mean the same effect. Your doctor must adjust the dose based on how the drug is released in your body. Self-switching can lead to under-treatment or overdose.
Final Takeaway
Extended-release and immediate-release aren’t just about convenience. They’re about safety, timing, and how your body handles medicine. One pill can be a lifeline. The same pill crushed or taken at the wrong time can be a trap. Always know what you’re taking, why you’re taking it, and how it’s built. When in doubt, ask your pharmacist. They’re trained to catch the details your doctor might not have time to explain.
Noah Fitzsimmons
Oh wow, another ‘medication is magic’ post. Let me guess - you also think your coffee’s ‘extended-release’ because you drank it at 7am and still feel buzzed at 3pm? 🙄
Real talk: if you can’t follow basic instructions like ‘don’t crush pills,’ maybe you shouldn’t be trusted with a toaster, let alone a prescription. I’ve seen people split OxyContin like it’s a Snickers bar. Congrats, you just turned your living room into an ER waiting room. The FDA didn’t invent ‘do not crush’ because they hate fun - they did it because people are idiots. And yes, I’m talking to you, Cliff.
Eliza Oakes
Okay but what if you’re a 72-year-old with gastroparesis and your ER metoprolol is just sitting in your stomach like a brick for 8 hours? You’re supposed to ‘wait 2-4 hours’ but your body’s basically on vacation? This whole ‘patience is part of the treatment’ thing sounds like a cult mantra. I had my dad take his ER gabapentin and he ended up in the hospital because the pill just… sat there. Then he got a double dose because he thought it wasn’t working. Now he’s on IR. And yes, he takes it 3x a day. And guess what? He’s alive. And not confused. So maybe the ‘one-size-fits-all’ advice is just as dangerous as crushing pills.
Clifford Temple
Americans are so soft. You people can’t even swallow a pill right? In my country, we don’t have ‘extended-release’ because we don’t need it - we take the damn pill and get on with life. No ‘breakthrough symptoms,’ no ‘osmotic pumps,’ no ‘polypills.’ Just medicine. And if you can’t handle it, maybe you shouldn’t be on it. This whole post reads like a pharmaceutical ad written by a kindergarten teacher. Crush it? Chew it? What’s next - microwave it? Get a grip. This isn’t a TED Talk. It’s a pill. Take it. Don’t overthink it. And stop blaming the drug for your laziness.
Corra Hathaway
YASSSS this is so important!! 🙌 I’ve been on ER sertraline for 3 years and I used to panic every time I didn’t feel ‘better’ after 2 hours - like, why isn’t this magic fairy dust?! 😅 But then I learned: it’s not supposed to be. It’s a slow-burn love story between your brain and the drug. 💌 Now I use IR for panic attacks and I’m basically a zen master. Pro tip: label your pill organizer ‘ER AM’ and ‘IR PRN’ - it changed my life. Also, if you crush your pills, you’re basically doing cocaine with your antidepressants. Just sayin’. 💊✨ #MedicationLiteracy #NoMoreCrushing
Paula Jane Butterfield
Hey everyone - I’m a pharmacist in rural Ohio and I see this ALL the time. People think if a pill has a score line, it’s okay to split - but Venlafaxine XR? Nope. The matrix inside isn’t uniform. You get 70% of the dose in one half, 30% in the other. That’s not dosing - that’s Russian roulette. I had a guy come in after crushing his Adderall XR because he ‘needed focus for finals.’ He had a heart rate of 140 and was hallucinating. We saved him. But he didn’t know any better. So please - if you’re unsure, ASK. Don’t Google it. Don’t Reddit it. Ask your pharmacist. We’re paid to know this stuff. And yes, we’ll help you even if you’re embarrassed. We’ve seen it all. 💙
Simone Wood
Extended-release is a corporate scam dressed up as science. Why does a 12-hour pill cost 20% more? Because they’re charging you for the *illusion* of convenience. My GP prescribed me ER bupropion because ‘it’s better for adherence.’ But I’m not a child - I can set an alarm. IR is cheaper, faster to titrate, and if I miss a dose, I don’t have to wait 8 hours for the next one. The whole ‘steady levels reduce side effects’ argument is bullshit - I had more nausea on ER because the drug just sat there and fermented in my gut. IR let me control the spikes. And I’m not alone. Ask anyone on r/Depression who’s tried both. The data’s skewed by pharma-funded studies. Trust your body, not the label.
Swati Jain
As someone from India where ER meds are often unaffordable, I’ve seen people split pills out of necessity - and yes, sometimes it works. But I’ve also seen people die because they didn’t know the difference. I work in a clinic where we teach patients to use a ‘pill calendar’ - draw a sun for morning ER, a moon for night, and a lightning bolt for IR PRN. It’s simple. No jargon. No tech. Just visuals. And guess what? Adherence jumped 60%. You don’t need a PhD to understand timing - you need clear communication. And yes, I’ve had patients cry because they thought crushing their pill was ‘clever.’ Please. Don’t be clever. Be safe.
Florian Moser
This is one of the clearest, most accurate explanations of ER vs. IR I’ve ever read. The table alone is worth a medical school lecture. The key takeaway - and I’ve said this to dozens of patients - is that timing isn’t optional. It’s pharmacological physics. A 36mg ER Adderall isn’t ‘36mg’ - it’s 36mg delivered over 12 hours. Crush it, and you’re ingesting a 36mg bolus. That’s not a dose - that’s a toxin. I’ve seen ER opioids cause respiratory arrest in elderly patients because their kidneys couldn’t clear the slow release fast enough. This isn’t opinion. It’s physiology. If you’re on ER meds, treat them like a time bomb that’s supposed to tick slowly - not like a grenade you can open to ‘get more bang.’ And yes, your pharmacist is your best friend. Talk to them.