Juvenile Arthritis Medication Guide
| Medication Type | How It Works | Typical Onset | Common Side Effects |
|---|---|---|---|
| NSAIDs | Reduces inflammation by blocking COX enzymes | Hours to days | Stomach upset, occasional headache |
| DMARDs | Modifies immune response to slow joint damage | Weeks to months | Nausea, liver enzyme changes, increased infection risk |
| Biologics | Targets specific cytokines (e.g., TNF-α) that drive inflammation | Days to weeks | Injection site reactions, rare infections |
Important Note: This tool provides general educational information only. Always consult with your healthcare provider for personalized medical advice regarding your specific condition and treatment plan.
Living with juvenile arthritis as a teenager feels like juggling school, friends, and a body that doesn’t always cooperate. The good news? You don’t have to figure it out alone. This guide breaks down the biggest hurdles-pain, fatigue, meds, school life, and mental health-and offers practical steps you can start using today.
What Is Juvenile Arthritis?
Juvenile Arthritis is a chronic inflammatory condition that begins before age 16 and causes joint pain, swelling, and stiffness. It comes in several sub‑types, the most common being oligoarticular (affecting four or fewer joints) and polyarticular (affecting five or more). About 300,000 children in North America live with this condition, and teens often experience flare‑ups that disrupt everyday activities.
Top Challenges Teens Face
- Unpredictable pain spikes that clash with class schedules.
- Morning stiffness that makes getting out of bed feel like a marathon.
- Fatigue that lingers even after a full night’s sleep.
- Social pressure to “act normal” while hiding medication bottles.
- Navigating school policies that may not understand your medical needs.
Managing Physical Symptoms
There’s no one‑size‑fits‑all solution, but pairing medication with lifestyle tweaks can keep flare‑ups in check.
Medication Basics
Doctors typically start with NSAIDs (non‑steroidal anti‑inflammatory drugs) to reduce pain and swelling. If symptoms persist, they may add DMARDs (disease‑modifying antirheumatic drugs), which work slower but target the disease process. For aggressive cases, Biologic therapies such as etanercept or adalimumab block specific immune pathways.
Pain‑Relief Strategies
- Apply heat before activity and cold packs after intense use.
- Use over‑the‑counter topical analgesics sparingly.
- Practice deep‑breathing or guided meditation for acute pain spikes.
Dealing With Fatigue
Schedule short, frequent breaks during homework or study sessions. A 10‑minute walk or gentle stretching can recharge energy levels without overexerting joints.
Medication Options: A Quick Comparison
| Medication Type | How It Works | Typical Onset | Common Side Effects |
|---|---|---|---|
| NSAIDs | Reduces inflammation by blocking COX enzymes | Hours to days | Stomach upset, occasional headache |
| DMARDs | Modifies immune response to slow joint damage | Weeks to months | Nausea, liver enzyme changes, increased infection risk |
| Biologics | Targets specific cytokines (e.g., TNF‑α) that drive inflammation | Days to weeks | Injection site reactions, rare infections |

Staying Active and Building Strength
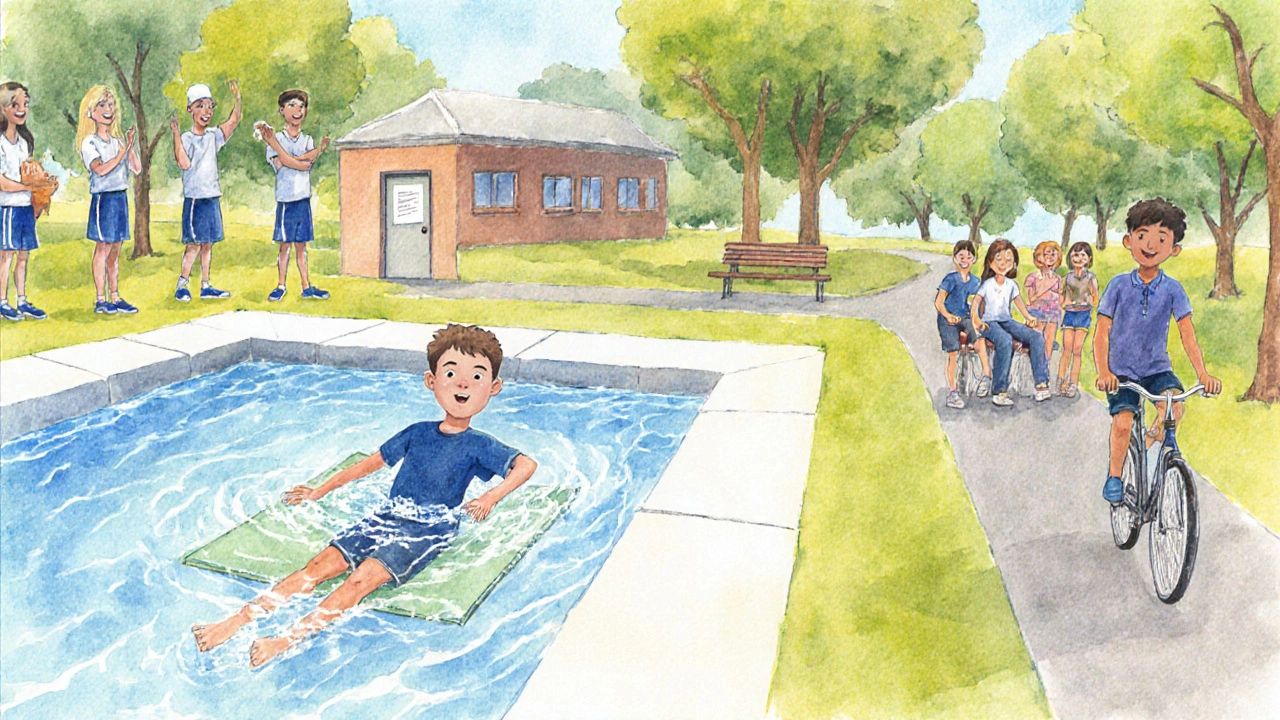
Exercise isn’t a luxury-it’s a core part of managing JIA. The goal is to keep joints moving without triggering pain.
- Physical therapy can teach joint‑protecting techniques and personalized stretching routines. \n
- Low‑impact activities like swimming, cycling, or yoga improve cardio fitness while sparing the knees and elbows.
- Strength training with light resistance bands helps support joints; aim for two 15‑minute sessions per week.
School and Social Life: Practical Hacks
School can feel like a battlefield when you’re dealing with unpredictable symptoms. Here’s how to make it work:
- Get a written plan from your pediatric rheumatologist outlining medication timing, needed breaks, and any mobility aids.
- Talk to a guidance counselor about school accommodations-extra time on tests, a private room for injections, or a locker close to your classroom.
- Use a discreet medication case; many teens keep their meds in a small zip‑lock bag inside a backpack.
- Schedule “energy‑saving” periods: block out 15 minutes after lunch for a short walk or stretch.
- Inform close friends about your condition so they can offer help during flare‑ups without making it a big deal.
Mental Health and Emotional Support
The emotional rollercoaster of JIA is real. Chronic pain can trigger anxiety, low mood, or feelings of isolation.
- Consider seeing a therapist who specializes in chronic illness; cognitive‑behavioral therapy (CBT) can reframe pain thoughts.
- Join a support group-online forums or local meet‑ups let you share experiences with peers who “get it.”
- Practice journaling. Tracking flare‑up triggers helps you and your doctor adjust treatment plans.
- Stay connected to hobbies that don’t rely heavily on joint use-music, drawing, or coding can provide a creative outlet.
Preparing for the Transition to Adult Care
By late teens, most patients shift from pediatric to adult rheumatology services. Early preparation eases the switch.
- Start discussing transition plans with your doctor at age 16.
- Gather a summary of your medical history: diagnosis date, medication list, recent lab results.
- Practice self‑advocacy-learn to describe your symptoms and ask questions without a parent in the room.
- Explore insurance coverage for adult specialists; some plans require a referral.
Resources and Next Steps
Here’s a quick checklist to keep you on track:
- Print your medication schedule and keep it in your locker.
- Schedule a yearly review with your pediatric rheumatologist to assess disease activity.
- Ask your school nurse about a pain‑management plan for gym class.
- Join at least one online community-e.g., the Juvenile Arthritis Association forum.
- Set a monthly “self‑check” day: note pain levels, fatigue, and mood in a journal.
Remember, living with juvenile arthritis is a marathon, not a sprint. Small, consistent steps add up to big improvements over time.
Frequently Asked Questions
Can I still play sports?
Yes-choose low‑impact options like swimming, cycling, or yoga. Talk to your physical therapist about modifying techniques to protect joints.
What should I do if I forget a medication dose?
Take it as soon as you remember if it’s within a reasonable time frame. If it’s close to the next dose, skip the missed one to avoid double‑dosing. Always confirm with your doctor’s instructions.
How can I talk to my teachers about my condition?
Request a brief meeting, bring a note from your rheumatologist, and outline specific needs-extra time, a place to store medication, or permission for short breaks during class.
Is it normal to feel sad or anxious about JIA?
Absolutely. Chronic conditions can affect mood. Seeking counseling, joining support groups, and staying active are proven ways to boost mental well‑being.
When should I consider switching medications?
If you experience persistent flare‑ups despite current treatment, or if side effects become hard to manage, discuss alternatives with your rheumatologist. Blood tests and imaging help guide the decision.

Iván Cañas
Great rundown! I especially appreciate the clear table comparing NSAIDs, DMARDs, and biologics – it makes picking the right med way less intimidating.
One tip that helped me was syncing medication times with school bells so I never miss a dose.
Jen Basay
Loved the section on low‑impact sports – swimming really saved my joints during a rough flare 😊. Keeping a simple stretch routine before class can also cut down morning stiffness.
Poorni Joth
i cant beleive some ppl think you should just push through the pain its not just "toughness" its a real disease! we need more awareness and schools should actually listen when kids request accommodations.
Alisa Hayes
The advice about planning a written medication schedule is spot on. Having it printed and tucked in your locker helps both you and the school nurse keep track without awkward conversations.
Mariana L Figueroa
Remember to stay hydrated especially when taking NSAIDs it helps protect your stomach and kidneys
mausumi priyadarshini
While the guide emphasizes swimming, one might argue that over‑reliance on water‑based exercises could actually limit bone density, which is crucial during the teenage growth spurt, so incorporating weight‑bearing activities, even if low‑impact, may be advisable.
Suzette Muller
It’s normal to feel isolated during a flare; connecting with an online support group can provide a sense of community and practical tips from peers who truly understand the daily challenges.
Manju priya
Implementing short, structured breaks during study sessions not only mitigates fatigue but also promotes joint mobility; a five‑minute walk every hour can dramatically improve focus and reduce stiffness.
Jesse Groenendaal
People need to stop ignoring the mental health side of JIA it’s as important as the physical symptoms
Persephone McNair
the neuro‑immune axis plays a key role in fatigue patterns especially during cytokine storms from biologics so monitoring biomarkers could inform personalized break schedules
scott bradshaw
Oh sure, just ignore the whole guide and wing it – that’s how champions are made.
Crystal Price
Life is a theater and JIA is the unseen script that forces us to improvise on every stage.
Murhari Patil
They don’t want you to know that the “new” biologics are part of a larger scheme to keep the pharma giants in power – vaccine‑like cycles disguised as treatment upgrades.
kevin joyce
Living with juvenile arthritis is not merely a medical condition, it is an existential challenge that forces a teenager to renegotiate identity and purpose. Each morning stiffness becomes a metaphor for the friction we encounter when society expects linear progress without acknowledging hidden impediments. The pharmacological arsenal-NSAIDs, DMARDs, biologics-serves as both shield and compass, guiding the body through turbulent inflammatory storms. Yet the true therapy lies in the cultivation of resilience, a practice cultivated through mindful awareness of breath and movement. When a teen decides to engage in low‑impact swimming, the water becomes a liminal space where gravity's grip loosens, allowing the joints a reprieve. Conversely, neglecting the psychosocial dimension can erode motivation, turning medication adherence into a mechanical ritual devoid of meaning. Integrating cognitive‑behavioral strategies transforms pain signals into data points, enabling a proactive dialogue with one’s own physiology. The school environment, often perceived as a rigid institution, can be reframed as a collaborative network if the student, caregiver, and educator co‑author an accommodation plan. Journaling, though seemingly simple, acts as a reflective surface where patterns of flare‑ups surface, informing both patient and clinician. Peer support groups function as echo chambers of shared experience, amplifying hope while attenuating isolation. Transitioning to adult care is akin to crossing a threshold, demanding both self‑advocacy and an awareness of evolving insurance landscapes. Preparing for this shift by compiling a concise medical summary is not just administrative diligence; it is an act of empowerment. The cumulative effect of these strategies is a gradual reconstitution of agency, allowing the teenager to navigate the marathon of chronic illness with intentional strides. Ultimately, the synthesis of medical, physical, and emotional interventions crafts a holistic paradigm that transcends the limitations imposed by juvenile arthritis. Embracing this integrated approach does not guarantee a painless journey, but it offers a roadmap toward a life defined not by disease, but by purposeful living.
michael henrique
Stop whining and follow the plan already.