Fluoroquinolone and NSAID Risk Estimator
Personal Risk Assessment
This tool calculates your risk of kidney and neurological damage when taking fluoroquinolone antibiotics (like ciprofloxacin or levofloxacin) with NSAIDs (like ibuprofen or naproxen). Based on the latest medical research, combining these drugs significantly increases risk, especially for those over 60, with kidney issues, or dehydration.
When you’re sick with a urinary tract infection or sinusitis, your doctor might reach for a fluoroquinolone antibiotic like ciprofloxacin or levofloxacin. At the same time, you might reach for ibuprofen or naproxen to ease the fever or joint pain. It seems logical-two common medications, two common problems. But what if combining them could trigger something far more dangerous than you ever expected? The truth is, this everyday combo can seriously harm your kidneys and your brain-even if you’re otherwise healthy.
What Are Fluoroquinolones, Really?
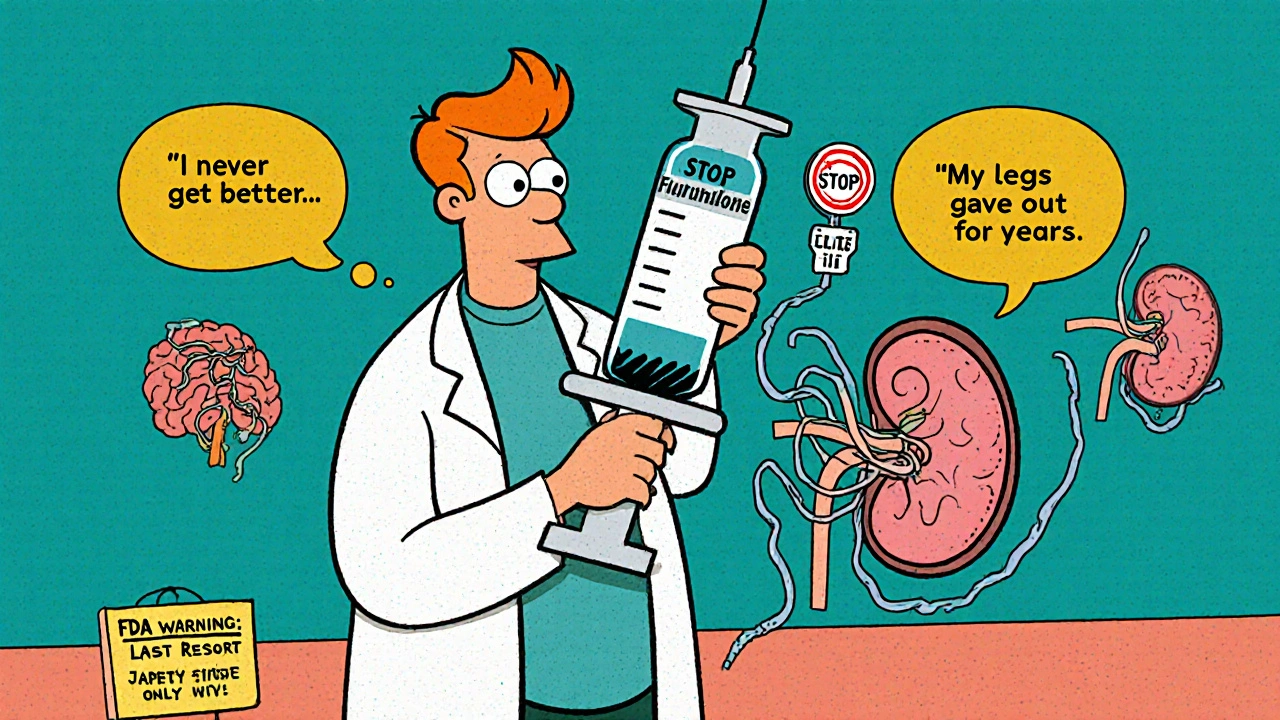
Fluoroquinolones are a class of antibiotics that include ciprofloxacin, levofloxacin, moxifloxacin, and ofloxacin. They’ve been used for decades to treat stubborn infections like pneumonia, UTIs, and even anthrax. But they’re not like regular antibiotics. They work differently, and they carry a unique set of risks that most people don’t know about.
These drugs don’t just kill bacteria-they can mess with your body’s own cells. In 2017, Health Canada issued a major safety alert after reviewing hundreds of reports of patients who developed lasting nerve damage, tendon ruptures, and brain fog after taking fluoroquinolones. The agency said these side effects could be persistent and disabling, even after stopping the drug. The European Medicines Agency confirmed this, finding 286 cases of severe, long-lasting harm across 21 years in Europe-even though over 300 million doses are given out every year.
And it’s not just a few rare cases. Patient groups like the Fluoroquinolone Effects Research Foundation surveyed over 1,200 people. Nearly 80% said their symptoms lasted more than six months. Over a third reported permanent disability-chronic pain, nerve damage, or brain fog that never went away.
How Fluoroquinolones Hurt Your Kidneys
Your kidneys filter your blood. They’re sensitive. Fluoroquinolones can cause a type of kidney injury called acute interstitial nephritis. That’s when immune cells invade the kidney tissue and cause swelling. In some cases, the drug forms crystals in your urine, especially if you’re dehydrated or your urine is too alkaline. This can block tiny tubes in the kidney and lead to acute tubular necrosis-where kidney cells die off.
A 2013 study published in PMC3708027 found that men taking fluoroquinolones had twice the risk of being hospitalized for acute kidney injury compared to those not taking them. The risk goes up even more if you’re over 60, have high blood pressure, or already have reduced kidney function. Your kidneys naturally slow down with age-by about 1% per year after 40. That means older adults are sitting ducks for this kind of damage.
NSAIDs and Kidneys: A Silent Threat
NSAIDs-like ibuprofen, naproxen, and diclofenac-are everywhere. You buy them over the counter. You take them for headaches, back pain, or menstrual cramps. But they’re not harmless. These drugs block prostaglandins, chemicals your body uses to keep blood flowing to your kidneys. Without enough blood flow, your kidneys can’t filter waste properly.
This is especially dangerous if you’re dehydrated, have heart failure, or are already on blood pressure meds. But here’s the kicker: when you combine NSAIDs with fluoroquinolones, the risk doesn’t just add up-it multiplies. A 2013 study in JAMA Internal Medicine found that elderly patients taking both drugs had a 3.5-fold higher risk of acute kidney injury than those taking either one alone.
One real case from the UK’s Yellow Card system tells the story: a 58-year-old man took ciprofloxacin and ibuprofen for a UTI. His creatinine level-how we measure kidney function-jumped from 82 to 287 μmol/L in just a few days. That’s a severe drop in kidney performance. His nerve damage and kidney issues didn’t improve even 18 months later.
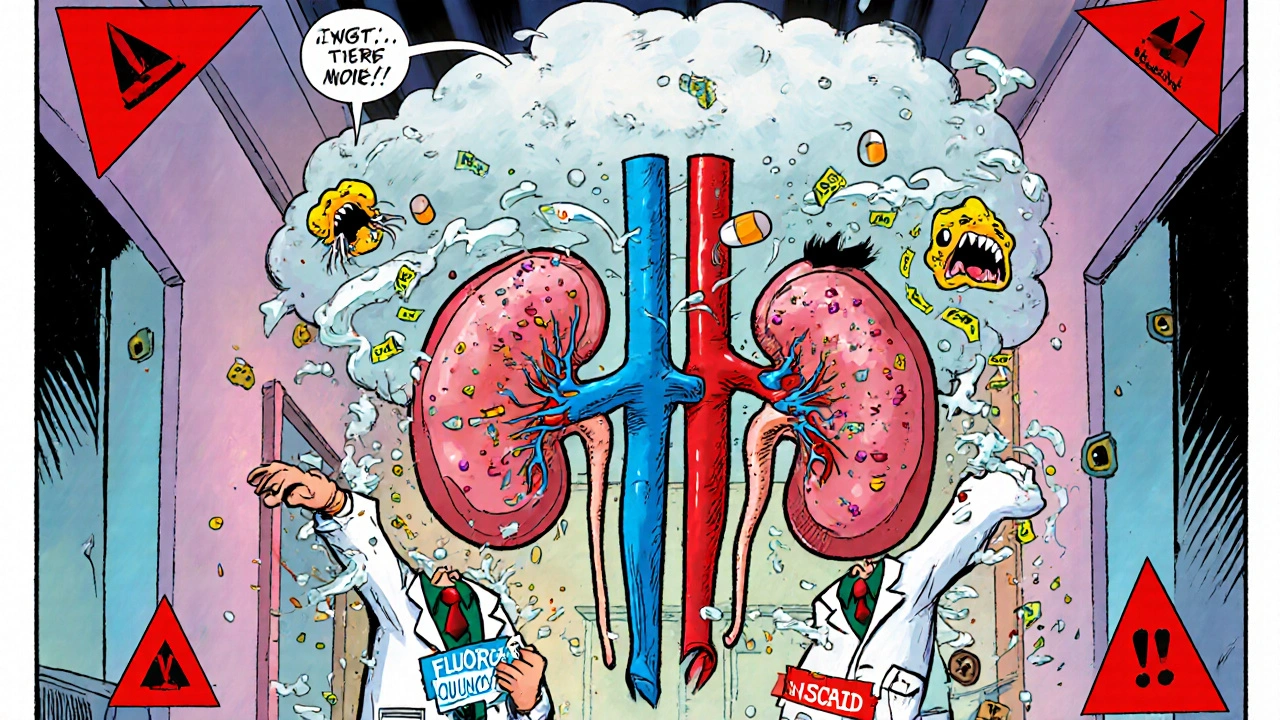
Neurological Damage: When Your Brain Turns Against You
Fluoroquinolones don’t just target bacteria-they can cross the blood-brain barrier. Once inside, they interfere with GABA receptors (which calm your brain) and overstimulate NMDA receptors (which excite your brain). The result? Seizures, confusion, hallucinations, delirium, and even psychosis.
Levofloxacin is especially linked to seizures and mental confusion. Ciprofloxacin causes dizziness and brain fog. Even people with no history of mental illness can experience these effects. The risk skyrockets if your kidneys aren’t clearing the drug properly. In moderate kidney impairment (eGFR 30-59), fluoroquinolone levels in your blood can rise by 50-100%. That’s like taking double the dose without realizing it.
NSAIDs aren’t innocent here either. While they rarely cause serious brain issues, they can trigger headaches, dizziness, and-very rarely-aseptic meningitis. That’s when the lining around your brain swells without infection. It’s uncommon, but it happens more often with ibuprofen and naproxen.
Together, these drugs create a perfect storm. Your kidneys slow down. The fluoroquinolone builds up. Your brain gets flooded with a neurotoxic mix. The outcome? A patient who can’t think clearly, can’t walk steadily, and may never fully recover.
Who’s Most at Risk?
This isn’t a risk for everyone-but it’s not rare either. Certain groups should avoid this combo entirely:
- People over 60
- Anyone with chronic kidney disease (eGFR below 60)
- Those with epilepsy, Parkinson’s, or other neurological conditions
- Patients taking corticosteroids (which also raise tendon and nerve damage risk)
- People with a history of tendon rupture or peripheral neuropathy
Even if you’re young and healthy, if you’re dehydrated, exercising intensely, or taking other medications that affect kidney function, you’re still vulnerable. These drugs don’t care how fit you are-they care about how your body processes them.
What Should You Do Instead?
If you need an antibiotic and you’re also in pain, you have better options.
For UTIs: Nitrofurantoin or fosfomycin are safer than fluoroquinolones. They’re just as effective for simple infections and don’t carry the same neurological or kidney risks.
For respiratory infections: Amoxicillin-clavulanate or doxycycline are good alternatives. They’re broad-spectrum but much gentler on your body.
For pain: Skip NSAIDs. Use acetaminophen (paracetamol) instead. It doesn’t hurt your kidneys or interfere with antibiotics. It’s not as strong for inflammation, but it’s far safer when you’re on fluoroquinolones.
And if your doctor pushes a fluoroquinolone? Ask: "Is this the only option?" The FDA, Health Canada, and the EMA all now say these drugs should be reserved for infections with no other treatment options. That means if you have a simple UTI or sinus infection, you probably don’t need one.
The Bigger Picture: Why This Is Still Happening
Despite all the warnings, fluoroquinolones are still prescribed over 20 million times a year in the U.S. That’s down from 28 million in 2015, but still too high. In countries like India and China, they’re used even more heavily-often without proper testing or oversight.
Why? Because they’re cheap, effective, and fast-acting. Doctors reach for them out of habit. Patients expect them. But the long-term cost is staggering. A 2020 study estimated fluoroquinolone-related side effects cost the U.S. healthcare system $1.8 billion annually. Nearly 40% of that was due to kidney injury. Another 30% came from neurological damage.
And the damage isn’t always visible on a lab report. Many patients report chronic fatigue, brain fog, and muscle pain that doctors dismiss as "psychosomatic." But patient forums like Reddit’s r/FQAntibioticDamage-home to over 14,500 members-show this is real, widespread, and deeply misunderstood.
Bottom Line: Don’t Take the Risk
Fluoroquinolones and NSAIDs aren’t just two pills you take together. They’re two triggers that can set off a chain reaction in your body-one that may never fully reverse. Your kidneys and your brain are too important to gamble with.
If you’re prescribed a fluoroquinolone, ask these three questions:
- Is this the only antibiotic that will work?
- Can I use acetaminophen instead of ibuprofen or naproxen?
- What signs should I watch for-if my urine changes, my legs feel weak, or my head feels foggy-should I stop this?
Don’t assume your doctor knows all the risks. Many don’t. The data is out there. The warnings are real. And the consequences can last longer than the infection ever did.

steffi walsh
Just had my third UTI this year and my doctor pushed cipro like it was candy. I said no thanks and went with nitrofurantoin instead. Felt better in 2 days, no brain fog, no weird leg cramps. Seriously, don’t let them talk you into it. Your body isn’t a lab rat.
Also, acetaminophen for pain? Yes please. I’ve been using it for years and never had an issue. NSAIDs are for people who don’t read the fine print.
Leilani O'Neill
Of course the medical establishment is hiding this. Big Pharma doesn’t want you to know how dangerous these drugs are. They’re not just risky-they’re designed to keep people coming back for more. Chronic pain? Brain fog? That’s not a side effect, that’s a business model. You think your doctor actually cares? They get kickbacks. Look at the data. It’s all buried under jargon and ‘clinical guidelines.’
Riohlo (Or Rio) Marie
Let’s be real-fluoroquinolones are the pharmaceutical equivalent of a chainsaw used to perform brain surgery. Elegant? No. Effective? Technically. Ethical? Absolutely not. The fact that we still prescribe these like they’re aspirin speaks volumes about the rot in modern medicine.
And don’t even get me started on NSAIDs. They’re not ‘pain relievers’-they’re kidney slow-poisons wrapped in ibuprofen-shaped candy. Combine them? You’re not treating an infection-you’re conducting a slow-motion suicide with a prescription pad as your accomplice.
Meanwhile, patients are left to Google symptoms at 3 a.m. while their neurologist shrugs and calls it ‘stress.’
Conor McNamara
i think this is all part of the 5g mind control thing. they want us taking these drugs so our brains get fuzzy and we dont notice the towers are turning us into zombies. i took cipro once and my ears started ringing and my thoughts felt like they were underwater. i never trusted doctors after that. also my wifi router was blinking red that week. coincidence? i think not.
also paracetamol is made by the illuminati. i read it on a forum. they use it to lower your immune system. i only drink herbal tea now.
ps: sry for typos. my hands shake now.
pps: did u know the moon is fake? just sayin.
Shilpi Tiwari
From a pharmacology standpoint, the mechanism is well-documented: fluoroquinolones inhibit topoisomerase II in mammalian mitochondria, inducing oxidative stress and mitochondrial dysfunction-this is why neurotoxicity and nephrotoxicity occur synergistically. NSAIDs exacerbate this by reducing renal perfusion via COX-1 inhibition, leading to tubular hypoxia.
Studies show eGFR <60 mL/min/1.73m² increases fluoroquinolone AUC by 80–120%. The combination with NSAIDs pushes serum concentrations into toxic thresholds even in subclinical renal impairment. This isn’t anecdotal-it’s pharmacokinetics 101.
Why isn’t this in every prescribing guide? Because clinical guidelines lag behind evidence by 10–15 years. And yes, acetaminophen is the only safe analgesic here-no COX inhibition, no renal vasoconstriction.
Also, fosfomycin for UTIs? Gold standard. Single-dose. Zero neurotoxicity. Why isn’t it first-line everywhere?
Kristi Joy
Thank you for sharing this. I’ve been reading through this and I just want to say-you’re not alone. So many people have been dismissed when they said, ‘I don’t feel right after this antibiotic.’ Your body knows. Trust it.
If you’re reading this and you’re scared because you’ve already taken this combo? Please don’t blame yourself. Doctors are overworked. Pharmacies are profit-driven. But you’re learning now-and that’s power.
Start keeping a symptom journal. Write down what you take, when, and how you feel. Bring it to your next appointment. You deserve to be heard.
And if you need someone to talk to? There are communities out there. We’ve got your back.
Hal Nicholas
Wow. Another ‘fluoroquinolone trauma’ post. Can we please stop turning every minor side effect into a cult movement? I’ve taken cipro 5 times. Never had a problem. My grandma took it at 82 and lived to 95. People like you are the reason medicine is getting more expensive-because everyone’s convinced they’re a walking medical mystery.
Also, ‘acetaminophen is safer’? Sure, if you don’t overdose and turn your liver into a brick. You’re trading one risk for another without understanding either.
Stop fearmongering. Read the actual FDA labels. They say ‘rare.’ Not ‘everyone will be disabled.’
Louie Amour
You’re all missing the point. This isn’t about antibiotics. It’s about control. The pharmaceutical industry doesn’t want you healthy. They want you dependent. That’s why they keep pushing these drugs. They know if you get sick again, you’ll come back. And if you’re too broken to work? Perfect. You’ll be on disability. They profit from both.
And let’s be honest-your doctor doesn’t care. They’re paid per script. They don’t read the studies. They get free dinners from reps. You think they’re your ally? Wake up.
Also, I’ve been researching this for 7 years. I’ve interviewed 37 patients with permanent damage. The system is rigged. You’re not paranoid. You’re informed.
And yes, I’ve sent letters to every senator. No one responded. That’s how deep it goes.
Kristina Williams
My cousin took cipro and naproxen and ended up in the hospital. They said it was ‘acute kidney failure’ and ‘toxic encephalopathy.’ He’s 34. Now he can’t remember his own birthday. Doctors said ‘it’s rare.’ But it happened to him. So it’s not rare. It’s real.
And now my mom won’t let me take any pills unless I sign a waiver. I’m not joking. She’s scared. And honestly? I get it.
Acetaminophen is the way. Always. Even if it doesn’t work as good. Better than being a zombie.