Trying to keep track of multiple medications can feel overwhelming. You’ve got pills for your blood pressure, your diabetes, your cholesterol, maybe some pain relievers, vitamins, and herbal supplements. Some you take in the morning, others at night. Some you take with food, others on an empty stomach. And if you miss one, you’re not sure what to do. You’re not alone. Nearly half of people taking chronic medications don’t take them as prescribed. But there’s a simple, powerful tool that changes everything: a medication action plan.
What Is a Medication Action Plan?
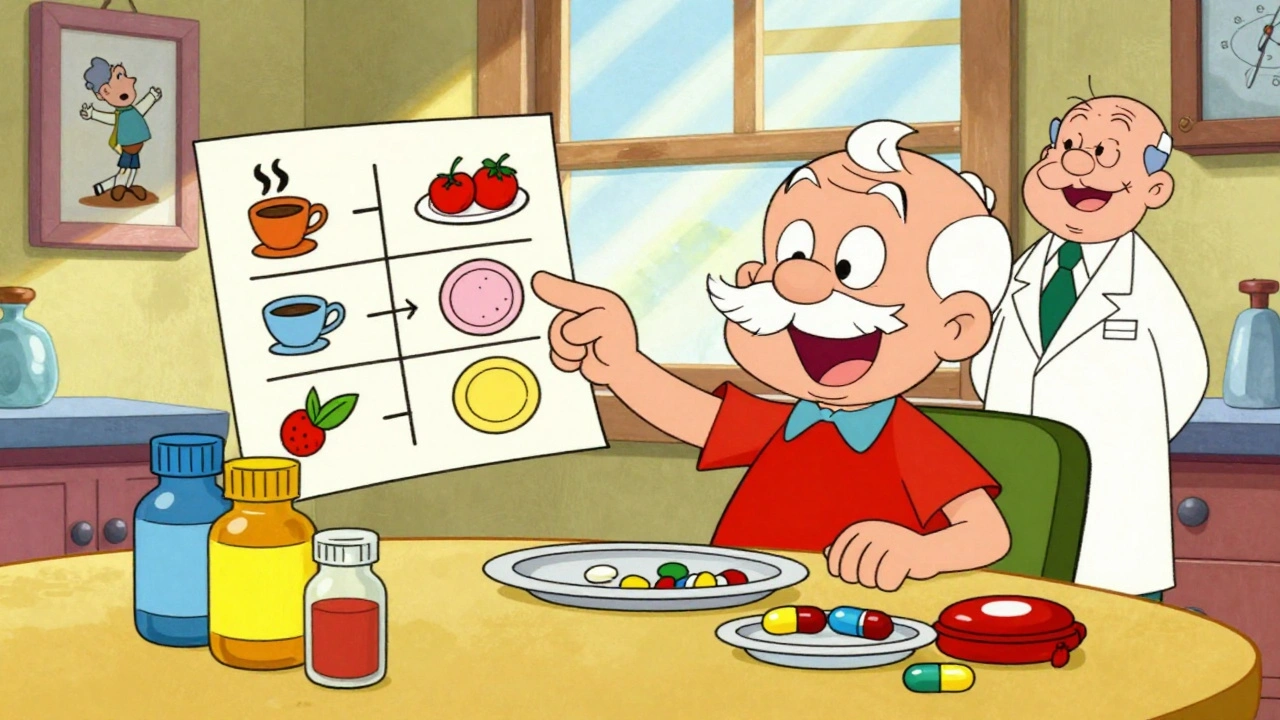
A medication action plan (MAP) isn’t just a list of your pills. It’s a personalized roadmap created with your care team - your doctor, pharmacist, nurse, or care coordinator - that tells you exactly what to do, when, and why. It turns confusion into clarity. Think of it as your daily instruction manual for staying healthy with your meds. Unlike a generic medication list you might get from the pharmacy, a true action plan includes specific steps tailored to your life. For example: "Take your metformin with breakfast, and if you skip breakfast, skip the dose." Or: "If your blood pressure reads over 150/90 two days in a row, call your pharmacist before taking your next dose of lisinopril." These aren’t vague suggestions. They’re clear, measurable actions. The concept isn’t new. Germany started requiring these plans for patients on three or more medications back in 2016. In the U.S., Medicare Part D has required them since 2006 for people taking eight or more chronic medications. But now, eligibility is expanding. By 2025, millions more Americans will qualify - including those on just five chronic meds. That means more people will be offered this tool. And if you’re managing multiple conditions, you deserve one.Why It Works: The Science Behind Better Adherence
People don’t miss doses because they’re lazy. They miss them because they’re confused, overwhelmed, or unsure what to do when things go wrong. A well-made action plan fixes that. Studies show that when patients help create their own medication action plan, adherence improves by 25% to 40%. That’s not a small number. It means fewer hospital visits, fewer emergency trips, and better control of conditions like diabetes, heart failure, and high blood pressure. One study found that patients with a personalized plan had 32% fewer medication-related hospitalizations in the year after getting it. The key? Personalization. A 2022 Johns Hopkins study found that patients given pre-printed, one-size-fits-all plans saw no improvement at all. But those who worked with their pharmacist to build a plan that matched their routine - like placing pills next to their toothbrush or setting phone alarms tied to meals - saw dramatic results. One woman with diabetes turned her plan into a visual chart: coffee cup for morning meds, dinner plate for evening ones. Her adherence jumped from 65% to 95%.Who Should Have One?
If you take three or more prescription medications regularly - especially for chronic conditions like diabetes, heart disease, COPD, or depression - you should have a medication action plan. It’s also critical if you:- Take over-the-counter meds or supplements daily
- See multiple doctors who prescribe different things
- Have trouble remembering when to take your pills
- Have had a recent hospital stay or ER visit due to a medication issue
- Are 65 or older and on Medicare Part D

How to Create Your Medication Action Plan
Making your plan isn’t something you do alone. It’s a conversation. Here’s how to get started:- Collect everything you take. Gather every pill, capsule, liquid, patch, inhaler, and supplement. Include over-the-counter drugs like ibuprofen, antacids, or sleep aids. Don’t forget vitamins, fish oil, or herbal teas you drink daily. Bring them all to your appointment - in the original bottles if possible.
- Schedule a Comprehensive Medication Review. This isn’t a quick chat. It’s a 30- to 60-minute session with your pharmacist or care coordinator. Ask your doctor to refer you, or call your pharmacy directly. Many offer these visits in person, over the phone, or via video.
- Ask the big questions. During your review, don’t be shy. Ask: "Why am I taking this?" "What happens if I skip it?" "What side effects should I watch for?" "What should I do if I feel worse?" Write these down ahead of time. Your care team needs to hear your concerns.
- Build the plan together. Your pharmacist will create a document with three parts: a list of all your meds (including dose and purpose), a list of problems (like too many pills, confusing schedules, or side effects), and a list of actions to fix them. For example: "Take metoprolol at 7 a.m. with breakfast. If you miss it, don’t double up. Take it only if it’s before noon. Call your doctor if your heart rate drops below 50."
- Make it visual and practical. If you’re more visual, ask for color coding: red for heart meds, blue for diabetes, green for pain. Use stickers, pictures, or a pill organizer with labels. Tie actions to daily habits - brushing teeth, eating lunch, turning off the TV. The more it fits into your life, the more you’ll stick with it.
- Get a copy you can carry. Ask for a printed version. Keep it in your wallet, purse, or phone. Update it every time your meds change - even if it’s just a new dose or a new pharmacy.
What Makes a Good Action Plan?
Not all plans are created equal. A strong one has these features:- Clear language. No medical jargon. "Take once daily" instead of "QD." "If you feel dizzy, sit down and call your pharmacist" instead of "Monitor for orthostatic hypotension."
- Measurable goals. Not "take your meds better." But "take all morning pills on 27 out of 30 days this month."
- Specific actions. Not "remember your pills." But "place your Monday-Wednesday-Friday pill box next to your coffee maker."
- Contingency plans. What if you’re sick? Traveling? Running out? A good plan tells you what to do.
- Updated regularly. Your plan should change when your meds change. Ask for a review every 3 to 6 months.
What to Do If You’re Not Given a Plan
You’re not stuck waiting for someone to offer you one. If you’re eligible and haven’t been offered a medication action plan, take action:- Call your pharmacy. Ask: "Do you offer Medication Therapy Management? Can I schedule a Comprehensive Medication Review?"
- Ask your doctor: "Can you refer me to a pharmacist for a medication action plan?"
- If you’re on Medicare Part D, you’re eligible if you take 8+ chronic meds or spend over $4,430 a year on prescriptions. Even if you’re not sure, ask.
- If you’re not on Medicare, check your private insurance website or call customer service. Many employers now include MTM as a benefit.

Real Stories, Real Results
One man in Halifax, 72, was taking 11 medications. He didn’t know why he took half of them. His blood pressure was all over the place. After a 45-minute session with his pharmacist, they created a color-coded plan with photos of each pill taped to a weekly chart. He tied each dose to a daily activity: morning coffee, lunch, bedtime. Within two months, his BP stabilized. He hasn’t been to the ER since. Another woman, 58, with rheumatoid arthritis and depression, was skipping her antidepressant because she felt it made her sleepy. Her plan didn’t just say "take daily." It said: "Take your sertraline at 8 p.m. with a snack. If you’re still tired after 3 days, call us - we may adjust the time or dose." She started taking it at night. Her energy improved. Her mood lifted. These aren’t miracles. They’re results of a simple, structured conversation.What’s Next for Medication Action Plans?
The future is digital. Apps are starting to sync with your MAP, sending reminders based on your schedule. Some can even flag potential drug interactions when you add a new OTC medicine. In 2024, new federal standards are rolling out to let your plan travel with you across hospitals, pharmacies, and clinics through electronic health records. But tech won’t replace the human touch. The most effective plans are still those built with someone who listens - a pharmacist who asks, "What’s stopping you?" not just "Did you take it?"Final Thought: You’re the Boss of Your Meds
Your medications are tools. A medication action plan is the instruction manual. And you’re the one who has to use them. No one else can do it for you. But you don’t have to figure it out alone. Your care team is there to help - if you ask. Start today. Gather your pills. Call your pharmacy. Ask for your plan. Write down your questions. Take the first step. Your health depends on it - and you’re closer than you think.Do I need a medication action plan if I only take a few pills?
Yes - even if you take just two or three medications, a plan can help. Many people don’t understand why they’re taking their pills or what to do if they feel side effects. A simple plan that explains the purpose of each med and what to do if you miss a dose can prevent mistakes and reduce anxiety. It’s not just for people with complex regimens.
Can my pharmacist really help me make a plan?
Absolutely. Pharmacists are medication experts trained in reviewing all your drugs - prescriptions, over-the-counter, and supplements - for interactions, duplications, and proper use. In many places, including Canada and the U.S., pharmacists can conduct formal Comprehensive Medication Reviews and create personalized action plans. You don’t need a doctor’s referral in most cases - just ask.
What if my plan uses medical terms I don’t understand?
Don’t accept it. A good plan uses plain language. If you see terms like "hypertension," "polypharmacy," or "QD," ask your pharmacist to rewrite them. Say: "I need this in words I can use every day." For example: "High blood pressure medicine" instead of "antihypertensive," or "take once daily" instead of "QD." Your understanding is the goal - not the jargon.
How often should I update my medication action plan?
Update it every time your meds change - new prescription, dose change, or stopping a drug. Even if nothing changes, review it every 3 to 6 months. Your body, lifestyle, or health needs might shift. A plan that worked last year might not fit now. Ask your pharmacist to schedule a quick check-in.
Can I use a digital app instead of a paper plan?
Yes - and many people find apps easier. Apps like MyTherapy, Medisafe, or your pharmacy’s own app can send reminders, track doses, and even share updates with your care team. But make sure the app is based on your official plan. Don’t rely on a generic med tracker. Your plan should be the source, and the app should follow it - not replace it.
What if I can’t afford my medications?
Cost is a major reason people skip doses. Your pharmacist can help. Many have access to patient assistance programs, generic alternatives, or coupons. Some pharmacies offer $4 generic lists. If your plan includes a med you can’t afford, tell your care team. They can often switch you to a lower-cost option or connect you with resources. Never stop a med because of cost - talk to someone first.
Can I share my medication action plan with family or caregivers?
Yes - and you should. If you have someone who helps you manage your meds, give them a copy. This is especially important if you live alone, have memory issues, or travel often. A caregiver who knows your plan can help you stay on track and recognize warning signs. Just make sure they understand it’s your plan - not theirs to change.
Next steps: Gather your meds. Call your pharmacy today. Ask for a Comprehensive Medication Review. Bring your list. Ask your questions. Walk out with a plan you can actually use. That’s how you take control.
Jamie Clark
Let’s be real - the system doesn’t care if you live or die, it just wants you to keep buying pills. This MAP thing? It’s just another corporate buzzword wrapped in a pretty infographic. They don’t want you to be healthy, they want you to be dependent. And don’t get me started on pharmacists ‘co-creating’ plans - they’re just glorified cashiers with a clipboard.
Keasha Trawick
OH. MY. GOD. This isn’t just a plan - it’s a LIFELINE wrapped in a color-coded, alarm-triggered, coffee-mug-aligned SYMBIOTIC HEALTH CEREMONY. 🌈💊 I mean, imagine your meds as a symphony - metformin as the violins at breakfast, lisinopril as the cello at dusk, and that one sketchy herbal tea you swear ‘helps’? The bassoon that no one asked for but somehow still shows up. This isn’t compliance - it’s ART. And I’m crying because someone finally gave me permission to treat my pills like sacred rituals, not chores.
Bruno Janssen
I tried one of these. Took me 45 minutes to explain to the pharmacist that I don’t care what the label says - I take my blood pressure med with whiskey because it makes the dizziness go away. She wrote it down. Didn’t change a word. Now I just skip the meds and drink more. At least I’m happy.
Deborah Andrich
I’ve been taking 7 meds for 12 years and never had a real plan until last month. My pharmacist sat with me for an hour, asked me what I was scared of, and then we drew stick figures on a napkin. Now I have a chart taped to my fridge with emojis for each pill. I take them. I feel seen. If you’re scared to ask for this - I get it. But you deserve to not feel like a walking pharmacy.
Tommy Watson
lol this is so cringe. who even wrote this? some pharma rep posing as a nurse? i took my pills for 20 years without a ‘plan’ and i’m still alive. also ‘color coding’? ugh. my grandma just used a pillbox with numbers. why does everything have to be a tiktok trend now? 🤡
Sheldon Bird
You got this. Seriously. Even if you start with just writing down your meds on a sticky note - that’s a WIN. I did it after my heart scare. Now I’ve got a whole binder with photos, alarms, and even a little ‘I did it!’ sticker for each week. You don’t need perfection. You just need to start. 💪❤️
Karen Mccullouch
They want you to trust the system? Nah. This is just another way to make you feel guilty for not being perfect. I’m American. I take my meds when I damn well feel like it. If I die early, at least I lived on my terms. 🇺🇸
nithin Kuntumadugu
hahahahah this is so fake. u know who made this? big pharma. they want u to take 12 pills a day so u keep buying them. the real problem? u dont need all these meds. they’re selling u fear. my cousin in delhi takes 2 pills and lives to 95. u think they’re giving u a ‘plan’? they’re giving u a leash. 🤫
sharon soila
Every human being deserves dignity in their healthcare. A medication action plan is not a luxury. It is a basic right. If you are managing multiple conditions, you are not failing - you are surviving. And asking for help is not weakness. It is courage. Please, reach out. You are not alone.
Constantine Vigderman
OMG I just did this yesterday!! I called my pharmacy and they set up a 30-min call with their med coach - she helped me realize I was taking my cholesterol pill at night instead of morning and that’s why I was so tired!! Now I’ve got it on my phone with a little bell and I even told my dog and he barks when it’s time 😂 I feel like a superhero. You can do this too!! 🎉💊
Cole Newman
you’re all missing the point. the real issue is that doctors don’t even know what they’re prescribing half the time. i had a guy give me 5 new pills last month and he didn’t even check my chart. this ‘plan’ is just a bandaid. what we need is a system that doesn’t let doctors prescribe like they’re playing monopoly.
kevin moranga
I’ve been helping my mom manage her meds for 5 years now. She’s 78, has diabetes, heart issues, and arthritis. We started with a notebook. Then we moved to a pill organizer. Then we made a little checklist with smiley faces for each day she got them all. Now she doesn’t just take them - she *looks forward* to her pill time. It’s become a ritual. She says it’s the only thing that makes her feel in control. And honestly? That’s the real win. Not the numbers on a chart - the peace of mind. You can do this. Start small. Celebrate the tiny victories. You’re not just managing meds - you’re reclaiming your life.
Alvin Montanez
Let’s be honest - this whole ‘medication action plan’ movement is just a distraction from the fact that our healthcare system is broken. People don’t miss doses because they’re confused - they miss them because they can’t afford them. They don’t need a color-coded chart - they need a single-payer system that doesn’t charge $800 for a 10mg pill. This article is a feel-good lie. It makes people think they’re in control when the real power is in the hands of insurance companies and pharmaceutical CEOs. Stop blaming the patient. Fix the system.
Lara Tobin
My dad just got his plan last week. He cried when the pharmacist wrote down why each pill mattered - he said no one ever explained it before. I just wanted to say thank you for writing this. It’s not just about pills. It’s about being heard.