When you switch from a brand-name pill to a generic version, your body shouldn’t react differently. The active ingredient is the same. The FDA requires generics to be bioequivalent. But for many people, something changes. They get headaches. Their muscles ache. They feel dizzy or tired. And it’s not because the medicine changed - it’s because their expectations did.
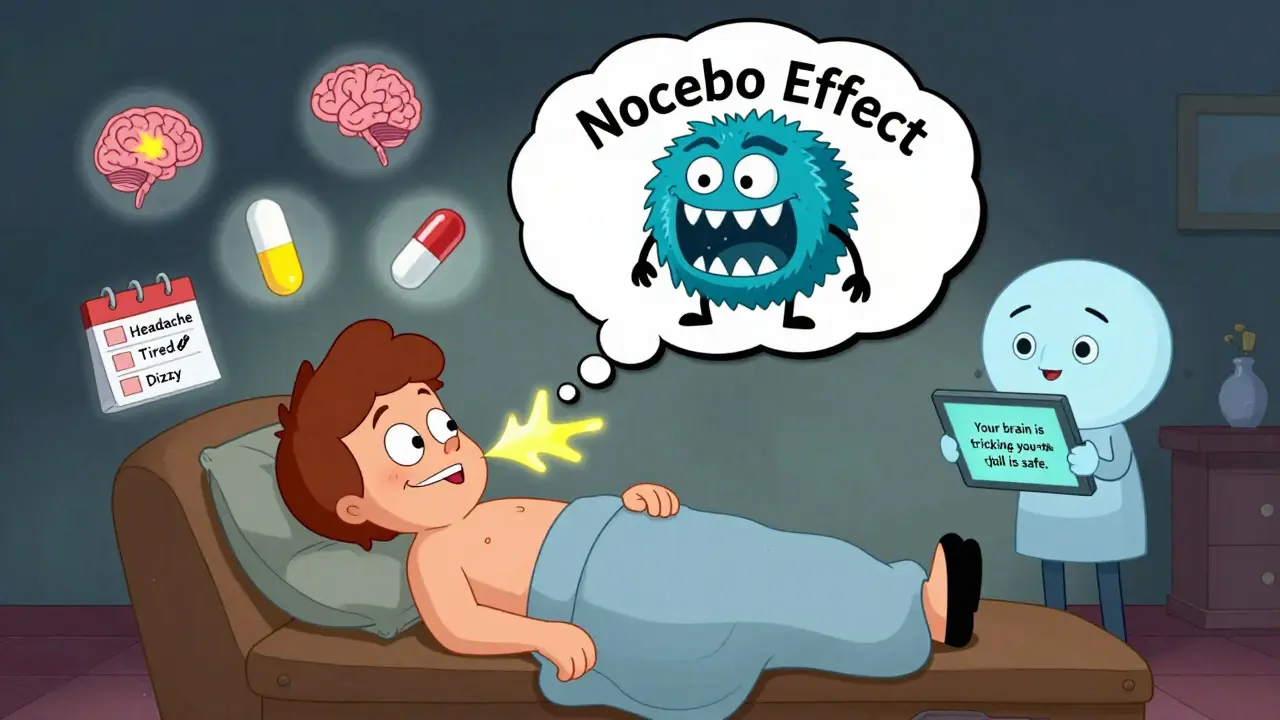
What Is the Nocebo Effect?
The nocebo effect isn’t a myth. It’s real biology. The word comes from Latin: nocebo means "I shall harm." It’s the dark twin of the placebo effect. Where placebo makes you feel better because you believe you’re getting help, nocebo makes you feel worse because you believe you’re going to suffer. In clinical trials, about 1 in 5 people taking sugar pills report side effects. About 1 in 10 quit the study because they think the medicine is making them sick. And here’s the kicker: those people aren’t imagining it. Their brains are activating pain pathways, raising stress hormones, and triggering real physical symptoms - all because they were told the drug might cause problems. This happens most often with generic medications. When patients hear, "This is the cheaper version," or worse, "It might not work as well," their brains start scanning for anything unusual. A normal ache? Must be the pill. A little fatigue? Must be the switch. A bad mood? Definitely the generic.Why Generics Trigger the Nocebo Effect
Generics look different. They’re a different color. Different shape. Different brand name. To most people, that’s enough to think they’re different inside - even when they’re not. A study in New Zealand showed this clearly. When patients switched from one brand of venlafaxine to a generic, reports of side effects stayed low - until the media started running stories about "problems with the new pill." Suddenly, reports spiked. The medicine hadn’t changed. The patients’ minds had. Doctors play a role too. If a prescriber says, "I know this isn’t the brand you used to take," or "Some people don’t tolerate the generic well," they’re planting the seed. One study found that when doctors used negative language about generics, patients reported 65% more side effects. When they said, "This works just as well and saves you money," side effects dropped by 37%. Even the packaging matters. Generic pills often come in plain white bottles. Brand-name drugs come in colorful, branded packaging. In one experiment, people given the same drug in a branded bottle reported better results than those given it in a plain bottle - even though the pills were identical.The Science Behind the Symptoms
It’s not just psychology. There’s real brain activity behind this. Brain scans show that when people expect pain or side effects, areas linked to anxiety and pain processing light up - even when nothing harmful is happening. In one study, patients told an epidural would feel like a "bee sting" reported much more pain than those told they’d feel "comfortable." Same needle. Same medicine. Different expectations. With statins, the most common complaint is muscle pain. But in double-blind trials, the rate of muscle pain is identical between people taking the real drug and those taking a sugar pill. That means for a lot of people, the pain isn’t from the statin - it’s from the fear of the statin. A 2023 study in The Lancet Digital Health tested an AI tool that personalized messages to patients switching to generics. It adjusted the tone based on their beliefs - reassuring those anxious about cost, explaining bioequivalence to those worried about quality. Result? A 41% drop in reported side effects.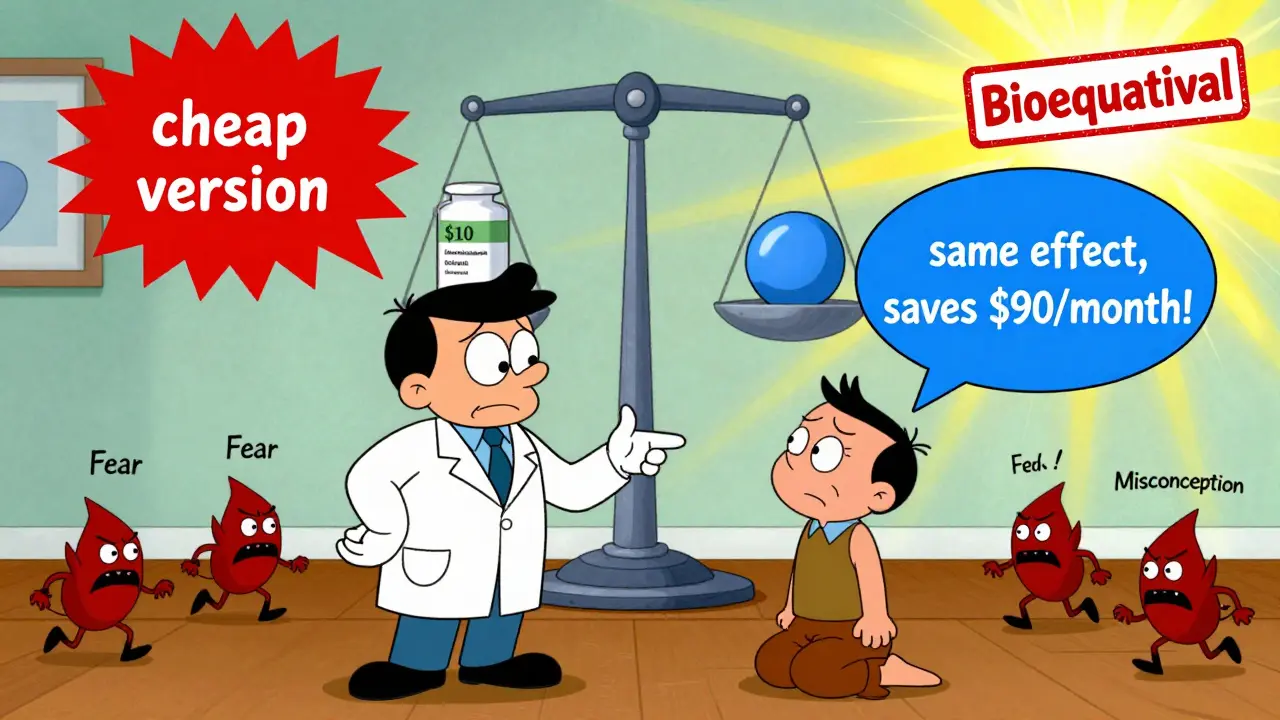
How the Nocebo Effect Costs You Money - and Health
This isn’t just about feeling bad. It’s about real consequences. In the U.S., 90% of prescriptions are filled with generics. But they make up only 24% of total drug spending. Why? Because people stop taking them. When someone stops a generic because they think it’s causing side effects, they often go back to the brand-name version. That costs $100 a month instead of $10. The U.S. healthcare system loses about $1.2 billion a year because of this. And it’s not just money. Stopping a medication because of a nocebo response can be dangerous. Someone with high blood pressure who quits their generic lisinopril because they think it’s making them dizzy might end up in the hospital. Someone with depression who stops their generic sertraline might relapse. A study in the Journal of Clinical Psychopharmacology found that 32% of patients switching from brand-name to generic antidepressants reported new side effects - compared to just 12% in the group told the switch was safe and effective.What Doctors and Pharmacists Can Do
The good news? This is fixable. Healthcare providers don’t need to lie. They just need to stop feeding fear. Here’s what works:- "This generic has the same active ingredient as your old pill. It’s been tested to work the same way."
- "Many people switch without any issues. If you notice something unusual, let’s talk - but it might not be the medicine."
- "This saves you $90 a month. That’s $1,000 a year you can use for groceries, gas, or a weekend away."
- Avoid saying: "This is the cheap version," or "Some people don’t do well with generics."
What You Can Do as a Patient
If you’ve switched to a generic and started feeling worse, pause before blaming the pill. Ask yourself:- Did I hear something negative about this switch - from a friend, a news story, or even my doctor?
- Are these symptoms new? Or could they be from stress, sleep loss, or something else?
- Did I feel fine on the brand-name version, or did I have these symptoms before?
waneta rozwan
Oh my god, I literally switched to generic Lexapro last year and started having nightmares and heart palpitations-I thought I was dying. Turns out? My brain was screaming "CHEAP DRUG = DANGER" and my body believed it. I went back to brand for a month just to prove it to myself... and guess what? Same exact symptoms. My mind was the problem. I feel so dumb but also so seen.
Nicholas Gabriel
Wow. This is so important. So, so important. And yet, so rarely discussed in medical training. I’ve seen patients quit statins because of muscle pain-only to find out, when we did a blinded rechallenge, they had zero issues with the placebo. The brain is a powerful, terrifying, beautiful thing. We need to teach this in med school. Like, yesterday. Please. Someone. Do something.
Cheryl Griffith
I’m a pharmacist and I’ve watched this play out a hundred times. A patient comes in furious because their generic blood pressure med "isn’t working"-but they’re sleeping 4 hours a night, drinking 3 coffees, and stress-eating tacos. I don’t say any of that. I just say: "Let’s check your numbers. And hey, this pill is literally the same as the one you were on. Same molecule. Same science. Same shot at feeling better." Sometimes, that’s all it takes. Just calm, clear facts. No drama.
swarnima singh
this is so true but also... we live in a world where everything is a scam right? like why should i trust a pill that looks like it came from a dollar store? the system is broken. the pharma companies are evil. the doctors are paid. the government is asleep. and now you want me to believe the cheap pill is the same? lol. i dont believe in anything anymore. except my own pain. and my pain is real. always.
Isabella Reid
As someone who’s been on generics for 8 years with zero issues, I just want to say: this isn’t about being gullible or weak. It’s about cultural conditioning. We’ve been sold the idea that expensive = better since birth. Ads, packaging, even the way doctors say "this is the brand-name version"-it all adds up. I think the real win here is not just better messaging, but a shift in how we value health. Not as a luxury product, but as a right.
Jody Fahrenkrug
My grandma switched to generic thyroid med and started feeling "off." We didn’t say anything. Just let her stay on it for two weeks. She came back and said, "I think I was just tired from gardening." No drama. No blame. Just time. Sometimes the fix is just... waiting for your brain to chill out.
Kasey Summerer
So let me get this straight: the placebo effect is real, but the nocebo effect is just "your brain being a drama queen"? 😂 I mean, I get it, but also… if your brain can make you feel pain with a sugar pill… then what’s the difference between that and a real side effect? Just semantics? 🤔
Corey Chrisinger
This is the most profound thing I’ve read all year. The nocebo effect isn’t just about pills-it’s about how we construct reality. We don’t just react to the world. We create it, in real time, from our fears, our stories, our media bubbles. A generic pill is just a mirror. It shows us what we already believe about value, trust, and safety. Maybe the real medicine isn’t in the capsule… it’s in the conversation.
Travis Craw
i used to hate generics til i got broke. now i use em all the time. never had a problem. but i do notice when my doc says "this is the cheap one" i get nervous. weird. so i just dont listen to that part. lol.
Christina Bilotti
Oh, so now we’re blaming patients for being too stupid to understand bioequivalence? How quaint. The real issue is that the FDA allows generics to vary by up to 20% in absorption rate-so yes, sometimes they’re not identical. And yes, some people are sensitive. But let’s not pretend this is just "psychology" while ignoring the fact that Big Pharma is happy to let you suffer so they can sell you the $100 bottle. This isn’t a nocebo-it’s a scam.
brooke wright
I switched to generic sertraline and started crying uncontrollably for 3 days. I thought I was going crazy. I told my doctor and she said, "It’s probably the pill." So I went back to brand. And I still cried. So I went to therapy. Turns out I was grieving my dad’s death and the pill just made me feel it. The pill didn’t cause it. But my fear made me think it did. I’m still on the generic now. And I’m okay.
vivek kumar
As someone from India, where generics are the only option for 90% of the population, I’ve never understood this fear. We’ve been using generics for decades. No one thinks they’re "inferior." They’re just medicine. The problem isn’t the pill-it’s the Western obsession with branding. You pay for logos, not efficacy. It’s absurd. And tragic.
Nick Cole
I work in ER. Saw a guy come in last month because he thought his generic metoprolol was "making him weak." He’d been on it for 6 months. Blood work? Perfect. BP? Normal. He was just tired from working two jobs. But he’d seen a TikTok video about "generic meds causing fatigue." That’s all it took. We gave him a pep talk and a new script. He left smiling. No meds changed. Just his mind did.