When you're on warfarin, your diet isn't just about what’s healthy - it’s about what’s consistent. A single meal of kale or spinach can throw your INR off balance, and that’s not a myth. It’s science. For people taking warfarin to prevent clots - whether after a heart valve replacement, for atrial fibrillation, or because of a history of deep vein thrombosis - managing vitamin K intake isn’t optional. It’s critical. And the good news? You don’t have to avoid vitamin K. You just have to keep it steady.
How Warfarin and Vitamin K Work Together
Warfarin doesn’t thin your blood. It slows down your body’s ability to make clotting factors. Specifically, it blocks an enzyme called VKORC1, which recycles vitamin K. Without enough active vitamin K, your liver can’t produce clotting factors II, VII, IX, and X. That’s how warfarin keeps your blood from clotting too easily.
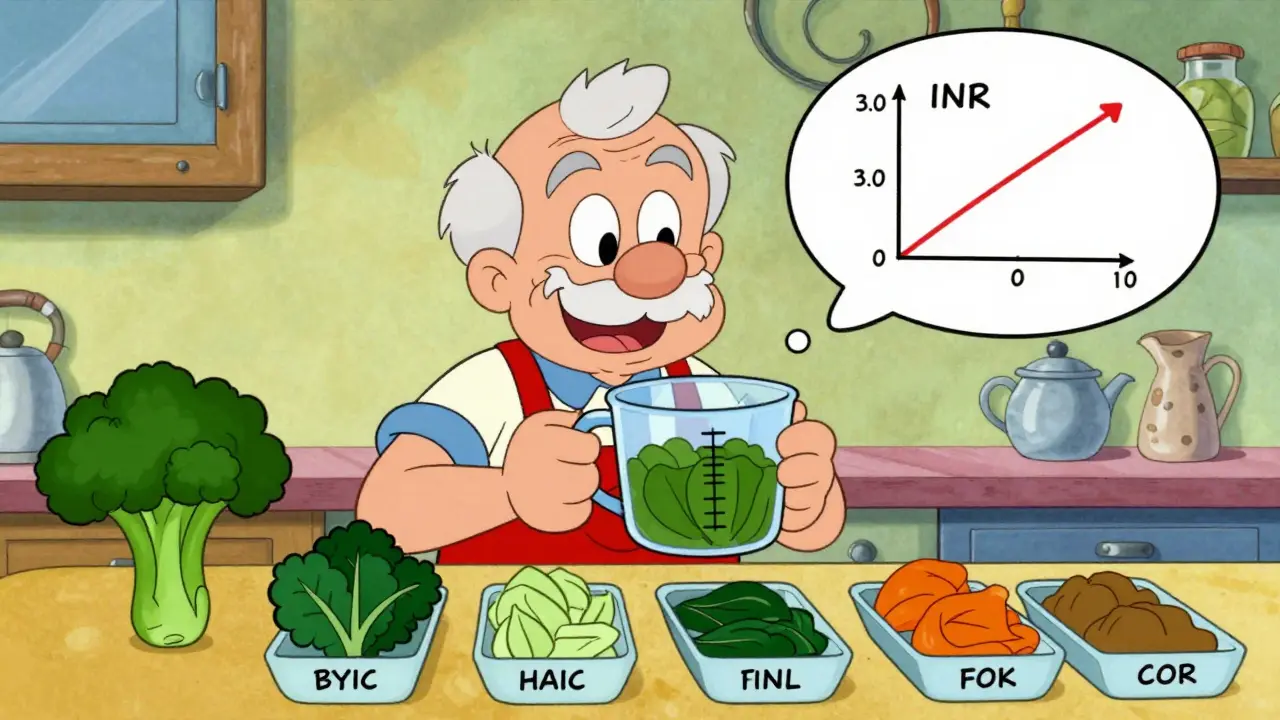
But here’s the catch: vitamin K from food fights back. Every time you eat a serving of broccoli, kale, or spinach, you’re giving your body more of the very thing warfarin is trying to block. If you eat a lot one day and almost none the next, your INR will swing wildly. High INR? You’re at risk of bleeding. Low INR? You’re at risk of clots. The target range for most people is 2.0 to 3.0. For those with mechanical heart valves, it’s often 2.5 to 3.5.
Which Foods Have the Most Vitamin K?
Not all vitamin K is the same. Phylloquinone (vitamin K1) is the main form in food, and it’s the one that affects warfarin. Menaquinones (K2) from cheese or natto don’t seem to interfere as much. So focus on K1 sources.
Here’s what you need to know about high-vitamin K foods:
- Spinach (cooked): 889 mcg per cup
- Kale (cooked): 547 mcg per cup
- Broccoli (cooked): 220 mcg per cup
- Brussels sprouts (cooked): 219 mcg per cup
- Swiss chard (cooked): 299 mcg per cup
- Parsley (raw): 246 mcg per 1/4 cup
On the other end, low-vitamin K foods include apples, bananas, carrots, potatoes, eggs, chicken, and white rice. These are safe to eat without worrying about INR swings.
Here’s the key: it’s not about avoiding these foods - it’s about eating the same amount every day. One cup of cooked spinach every day? Fine. One day with spinach, the next with iceberg lettuce? That’s a problem.
What Happens When You Change Your Diet?
Real patients see this every day. A Reddit user from Toronto reported her INR dropped from 2.8 to 1.9 after eating a large kale salad. Her doctor had to increase her warfarin dose by 20%. Another patient in Alberta saw his INR spike to 4.1 after switching from spinach salad to iceberg lettuce - a change from 145 mcg to just 17 mcg per serving. He almost bled internally.
These aren’t rare cases. A 2022 survey by the Blood Clot Organization found that 78% of warfarin users linked their INR fluctuations to diet changes. And 68% of all INR instability events were tied to dietary shifts - not medication errors, not alcohol, not illness. Just food.
Even small changes matter. A study in Thrombosis and Haemostasis showed that people who ate more than 250 mcg of vitamin K daily needed 17% more warfarin than those eating under 150 mcg. That’s a big difference in dose - and it’s all because of what they had for lunch.
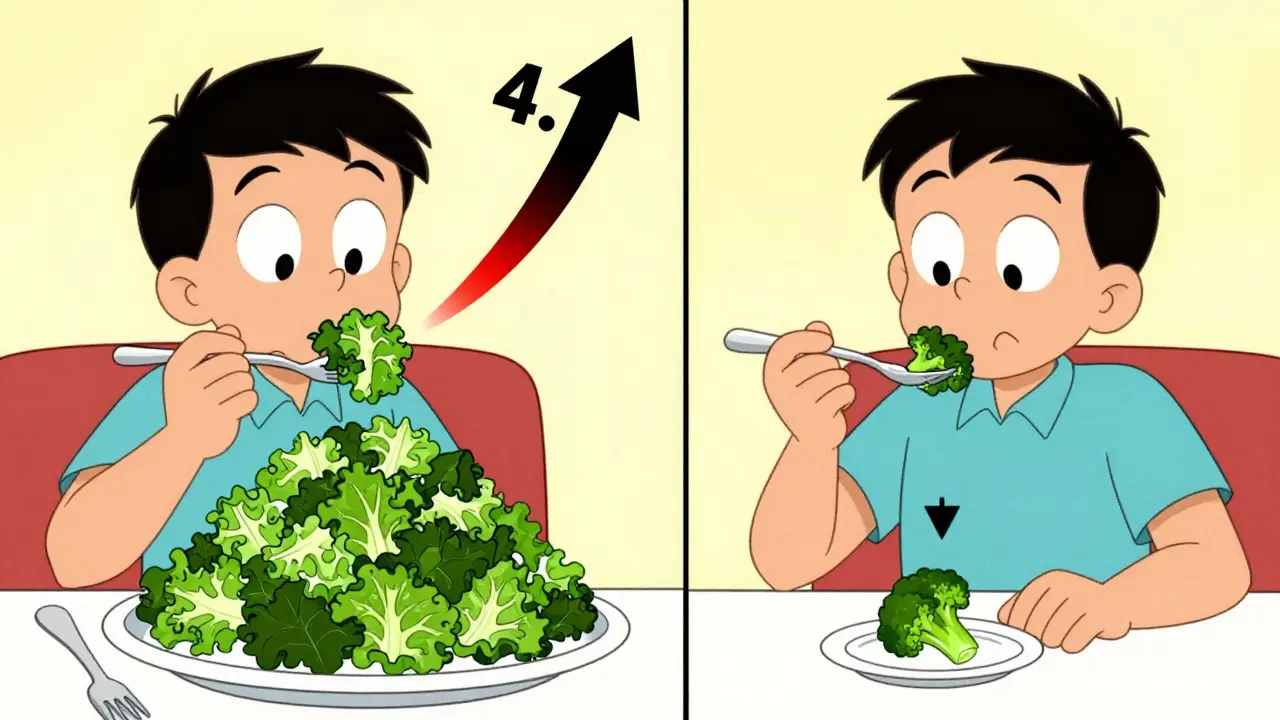
Consistency Is the Only Rule
The American College of Chest Physicians updated its guidelines in 2023: Don’t restrict vitamin K. Maintain it. That’s the new standard. You don’t need a low-vitamin K diet. You need a consistent one.
Experts recommend keeping your daily vitamin K intake within 10-15% of your usual amount. If you normally eat one cup of cooked broccoli (220 mcg), stick to that. Don’t double it. Don’t skip it. Don’t swap it for kale unless you’re ready to adjust your warfarin dose.
Here’s how to make it work:
- Choose one or two high-vitamin K foods you like and eat them daily. Broccoli? Great. Spinach? Fine. Just pick one and stick to it.
- Use a food scale or measuring cup. A “handful” of spinach isn’t the same as a “serving.” One cup cooked = 889 mcg. Half a cup = 445 mcg. Be precise.
- Track your intake. Apps like CoumaDiet (rated 4.6/5 by over 1,200 users) let you log meals and calculate vitamin K. Some clinics even use them to adjust doses remotely.
- Plan meals ahead. If you know you’re eating out on Friday, adjust your home meals earlier in the week to balance it out.
What About Cooking and Portion Size?
How you prepare food changes vitamin K levels. Boiling spinach cuts vitamin K by 30-50%. Steaming keeps more of it. Raw kale has more than cooked. So if you switch from raw kale to steamed broccoli, you’re not just changing food - you’re changing your dose.
Also, portion size matters. One cup of cooked spinach isn’t the same as two. And don’t assume restaurant portions are standard. A “side salad” at a diner might have three cups of greens - that’s over 2,500 mcg of vitamin K. That’s like taking a whole week’s worth in one meal.
When to Use Vitamin K Supplements
Some patients get stuck in a cycle: their INR keeps going too high, and their doctor keeps lowering their warfarin. But the real issue? They’re eating less vitamin K than they used to. Maybe they stopped eating greens because they were told to “avoid” them.
Here’s what works: low-dose vitamin K supplements. A study in the Journal of Thrombosis and Haemostasis found that giving patients 100-200 mcg of oral vitamin K daily helped stabilize INR in 83% of cases within a week. It’s not a cure - it’s a tool. If you’ve been eating less vitamin K than usual, a daily supplement can help bring your levels back into balance.
But don’t take it without talking to your provider. This isn’t something to self-prescribe.
Why DOACs Aren’t the Answer for Everyone
You’ve probably heard about newer blood thinners like apixaban or rivaroxaban. They don’t interact with vitamin K. So why not switch?
Because they’re not right for everyone. For people with mechanical heart valves - especially in the mitral position - warfarin is still the only approved option. Over 98% of these patients stay on warfarin. Same for antiphospholipid syndrome - 87% use warfarin. And for some older adults, warfarin is cheaper and more predictable than DOACs.
Even though DOACs make up 68% of new prescriptions, warfarin isn’t going away. In fact, the American Heart Association says it will remain essential for at least the next 15 years. That means learning to manage vitamin K isn’t a chore - it’s a skill you need to keep.
Tools and Support You Can Use
You’re not alone. Anticoagulation clinics across North America now offer:
- Registered dietitians trained in anticoagulation (available at 72% of U.S. clinics)
- Structured education programs that cut INR instability by 37%
- Mobile apps that track vitamin K and predict INR changes
- Monthly INR testing - the standard of care
Some clinics are even testing AI tools that look at your food logs and predict your next INR with 89% accuracy. It’s not science fiction. It’s happening now.
What to Do Today
If you’re on warfarin, here’s your action plan:
- Find out how much vitamin K is in your usual meals. Use a reliable source like the USDA FoodData Central or CoumaDiet.
- Identify your top 2-3 high-vitamin K foods. Pick one to eat daily - no more, no less.
- Measure your portions. Use a measuring cup. Don’t guess.
- Log your meals for a week. Look for patterns.
- Talk to your pharmacist or anticoagulation clinic. Ask if they offer diet counseling.
It’s not about perfection. It’s about predictability. Your body responds to consistency. And when your vitamin K intake is steady, your INR will be too.
Can I eat leafy greens while on warfarin?
Yes - but only if you eat the same amount every day. Leafy greens like spinach, kale, and broccoli are high in vitamin K, which directly affects how warfarin works. Eating them consistently - for example, one cup of cooked spinach every day - helps keep your INR stable. Switching between high and low vitamin K foods causes INR swings, which can be dangerous.
Does cooking reduce vitamin K in vegetables?
Yes, cooking can reduce vitamin K content - especially boiling. Boiling spinach or kale can cut vitamin K by 30-50%. Steaming, sautéing, or eating raw preserves more. That’s why it’s important to be consistent not just with what you eat, but how you prepare it. If you usually eat steamed broccoli, don’t suddenly switch to boiled broccoli without adjusting your warfarin dose.
Should I take a vitamin K supplement to help my INR?
In some cases, yes - but only under medical supervision. For patients with erratic diets or persistently high INR, a daily low-dose supplement (100-200 mcg) has been shown to stabilize INR in 83% of cases within a week. However, this is not a general recommendation. Taking supplements without knowing your current intake can make your INR unstable. Always talk to your doctor or anticoagulation clinic before starting any supplement.
Why can’t I just switch to a newer blood thinner like Eliquis or Xarelto?
Newer blood thinners (DOACs) don’t interact with vitamin K, which is a big advantage. But they’re not suitable for everyone. For example, people with mechanical heart valves - especially in the mitral position - must stay on warfarin because DOACs are not approved or effective for this condition. Also, warfarin is often cheaper and more predictable for older adults or those with certain medical conditions like antiphospholipid syndrome. Your doctor will recommend the best option based on your health needs.
How often should I get my INR checked?
Monthly INR checks are the standard of care for people on warfarin. When you first start, you may need checks every few days or weekly until your dose is stable. Once you’re consistent with your diet and medication, monthly checks are usually enough. But if you change your diet, start new medications, get sick, or travel, your provider may ask you to check more often. Always follow your clinic’s recommendations.
Managing vitamin K while on warfarin isn’t about fear. It’s about control. You’re not giving up your favorite foods - you’re learning how to use them wisely. With consistency, your INR will stay where it needs to be - and you’ll stay safe.