Antihistamine Driving Safety Calculator
This tool helps you understand how different antihistamines affect your driving ability compared to alcohol impairment levels. First-generation antihistamines can impair driving as much as having a blood alcohol level of 0.08% (the legal limit in most places).
Your Driving Safety Assessment
Select an antihistamine to see how it affects your driving ability
Key Recommendations
- If you're taking a first-generation antihistamine, don't drive for at least 4-6 hours after taking it.
- Second-generation antihistamines may cause impairment in 15-20% of users, especially at higher doses.
- Third-generation antihistamines like Fexofenadine (Allegra) and Levocetirizine (Xyzal) are the only ones proven safe for driving in multiple studies.
Antihistamines Can Slow You Down-Even If You Don’t Feel It
Many people take antihistamines without thinking twice. A runny nose? A sneezing fit? Pop a pill. But if you’re getting behind the wheel afterward, you might be putting yourself and others at risk-even if you feel perfectly fine. First-generation antihistamines like diphenhydramine (Benadryl) and chlorpheniramine are designed to block histamine, but they also cross into your brain, slowing down your reaction time, dulling your focus, and making you drowsy. Studies show these drugs can impair driving as much as alcohol. And the scary part? Most people don’t realize they’re impaired.
Not All Antihistamines Are the Same
There are three types of antihistamines, and their effects on driving vary wildly. First-generation antihistamines-like diphenhydramine, hydroxyzine, and clemastine-are the most sedating. They’re cheap, widely available, and often found in nighttime cold and allergy meds. But they’re also the most dangerous behind the wheel. On-the-road tests show they cause 30-50% more lane drifting than a sober driver, which is equivalent to having a blood alcohol level of 0.05% to 0.08%-the legal limit in most places.
Second-generation antihistamines like cetirizine (Zyrtec) and loratadine (Claritin) were developed to be less sedating. But don’t assume they’re safe. Cetirizine still causes measurable impairment in 15-20% of users, especially at higher doses. Loratadine is generally safer, but even it can affect reaction time in sensitive individuals. The labels say “non-drowsy,” but that doesn’t mean “no effect.”
Third-generation antihistamines-fexofenadine (Allegra) and levocetirizine (Xyzal)-are the only ones proven safe for drivers. In 16 double-blind studies using real driving tests, these drugs showed no significant difference from placebo. They barely enter the brain, so they don’t cause drowsiness, slowed thinking, or delayed reflexes. If you drive regularly and have allergies, switching to one of these is the smartest move you can make.
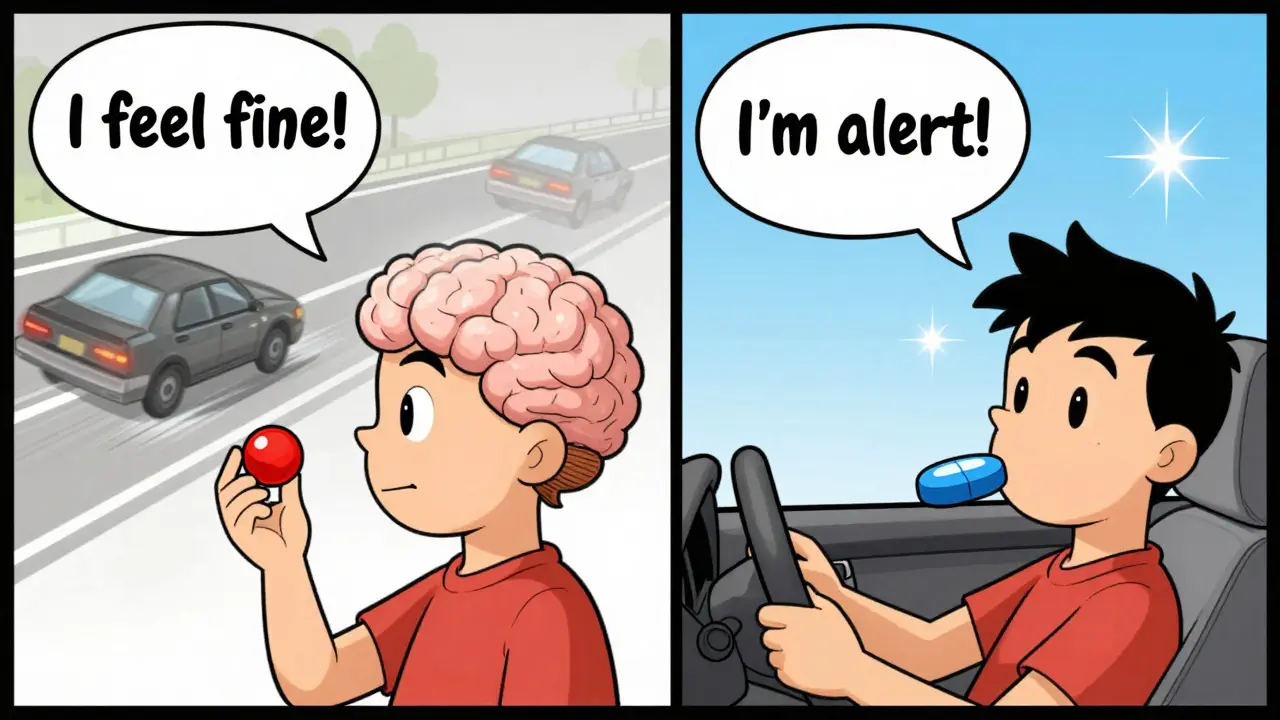
The Hidden Danger: You Don’t Feel Drowsy, But You’re Still Impaired
One of the biggest myths is that if you don’t feel sleepy, you’re fine to drive. That’s false. Research shows 70% of people who take first-generation antihistamines cannot accurately judge how impaired they are. You might think you’re alert, but your brain is processing information slower. Your eyes aren’t tracking as well. Your decision-making is delayed. A 2022 study from Ford’s Driving Skills for Life program found that drivers on these meds had slower responses to sudden stops, missed traffic signs, and struggled with lane changes-even when they insisted they felt fine.
It’s not just about sleepiness. Antihistamines can cause brain fog, reduced concentration, and poor hand-eye coordination. These aren’t obvious symptoms. You won’t yawn or nod off. But your ability to react to a child running into the street? That’s compromised. And that’s when accidents happen.
Alcohol Makes It Worse-Way Worse
Combining antihistamines with alcohol is like pouring gasoline on a fire. A single drink with a first-generation antihistamine can double or even triple your impairment. One study showed drivers who took diphenhydramine and had one beer performed worse than those who drank three beers alone. The effects aren’t just additive-they’re multiplicative. Even if you only have one glass of wine with dinner, avoid taking Benadryl afterward. Same goes for sleep aids, muscle relaxers, or any medication with a warning about drowsiness.
Legal Risks Are Real-And Growing
In Canada, you can be charged with impaired driving for taking any medication that affects your ability to operate a vehicle safely-even if it’s legal and prescribed. Police don’t need to prove you’re drunk. If a blood test shows antihistamines in your system and you’re involved in a crash, you could face fines, license suspension, or even criminal charges. In Europe, 22 countries have laws that ban driving for 8-12 hours after taking sedating antihistamines. In the U.S., over 3.5 million traffic violations each year involve impairing medications, and antihistamines make up 15-18% of those cases.
Insurance companies also take notice. If you’re in an accident and antihistamines are detected, your claim could be denied. Courts have ruled that knowingly driving while impaired by medication is negligence. You’re not just risking your life-you’re risking your legal standing, your insurance, and your future.
What Should You Do? A Simple Action Plan
- Switch to fexofenadine or levocetirizine. These are the only antihistamines proven safe for drivers. They work just as well for allergies but won’t slow you down.
- Never take first-gen antihistamines before driving. Even if you’ve taken them before and “felt okay,” your body can react differently each time.
- Test new meds at home. If you’re trying a new antihistamine, take your first dose at night. Wait 24-48 hours. See how you feel during normal tasks-reading, cooking, walking. Only then consider driving.
- Avoid nighttime driving after any antihistamine. Your body’s natural drowsiness at night combines with medication effects. This is when accidents spike.
- Check labels carefully. Look for “drowsiness” or “may cause sleepiness” warnings. If it’s not clear, call your pharmacist.
Cost Shouldn’t Be an Excuse
Yes, fexofenadine and levocetirizine cost more than Benadryl. A month’s supply of generic diphenhydramine runs about $4. The safer options? Around $35. But consider this: a single traffic accident caused by drowsy driving can cost tens of thousands in medical bills, legal fees, and lost wages. Insurance premiums go up. Your license could be suspended. The real cost isn’t the pill-it’s what happens if you get behind the wheel and your reaction time is off.
Many pharmacies offer discount programs. Ask if your plan covers third-generation antihistamines. Some generic versions of fexofenadine are now under $20 a month. That’s less than a tank of gas. And it’s the difference between getting home safely and ending up in a hospital.

Real People, Real Stories
On Reddit’s r/Allergies, one user wrote: “Took Benadryl before a road trip and had to pull over three times because I kept nodding off-never doing that again.” Another said, “I thought Zyrtec was safe. Then I almost ran a red light. My husband had to take over.”
Conversely, users who switched to Allegra report a different experience: “I drive 90 minutes to work every day. Took Allegra for the first time and didn’t feel a thing. Finally, I can manage my allergies without fear.”
These aren’t outliers. They’re data points. And they’re telling you something important: the right antihistamine makes all the difference.
What Doctors Are Saying
The American Academy of Allergy, Asthma & Immunology explicitly recommends third-generation antihistamines for anyone who drives, operates machinery, or works in safety-sensitive jobs. In 2022, 78% of allergists in the U.S. started prescribing fexofenadine or levocetirizine as their first choice for patients who drive.
Dr. F. Estelle R. Simons, a leading allergy expert, put it plainly: “Clinical tolerance to sedation is a myth. Just because you’ve taken it for years doesn’t mean your brain has adapted. The impairment is still there.”
Future Changes Are Coming
Regulators are catching up. In 2023, the European Medicines Agency required all antihistamine labels to clearly state driving risks based on generation and chemical class. The FDA is pushing for similar updates. Some U.S. states are considering mandatory screening for antihistamine use during driver’s license medical exams-especially for commercial drivers.
Meanwhile, new peripherally-acting antihistamines are in clinical trials. These drugs aim to block allergies without touching the brain at all. But until they’re available, stick with what’s proven: fexofenadine and levocetirizine.
Bottom Line: Drive Safe. Choose Smart.
If you have allergies and drive, your medication choice isn’t just about comfort-it’s about survival. First-generation antihistamines are outdated for anyone behind the wheel. They’re dangerous, legally risky, and unnecessary. Third-generation options are effective, safe, and widely available. Switching costs a little more, but it’s the only responsible choice. Don’t wait for an accident to make you rethink your meds. Your brain, your license, and your life are worth more than a $4 bottle of Benadryl.

Stacey Smith
This is why America is falling apart. People take pills like candy and then get behind the wheel like it's no big deal. No one takes responsibility anymore.
mukesh matav
I've been on Zyrtec for years and never had an issue. But I always wait a few hours after taking it before driving. Better safe than sorry.
Sarah Williams
Thank you for this. I switched to Allegra last year and my daily commute finally feels safe again. So many people don't realize how dangerous those old meds are.
Ben Warren
The empirical data presented in this article is unequivocally compelling. The pharmacokinetic profile of first-generation antihistamines demonstrates a statistically significant impairment in psychomotor performance, as corroborated by multiple peer-reviewed driving simulation studies. The assertion that subjective alertness correlates with objective driving competency is not only fallacious but dangerously misaligned with neurocognitive research. One must exercise rigorous epistemological discipline when evaluating self-reported wellness metrics in the context of pharmacologically induced central nervous system depression.
Grace Rehman
We treat our bodies like cars you can just refill with whatever's on sale at the gas station
But your brain isn't a fuel tank it's a supercomputer running on batteries that got swapped for knockoff ones
And somehow we're surprised when it freezes mid-drive
It's not about being tired it's about your neurons taking a nap while your ego thinks it's awake
And yeah I know you took Benadryl last Tuesday and lived
But your body doesn't remember it was a Tuesday
It just remembers the dose
And your brain doesn't care if you feel fine
It just cares if it can still process the color red before the kid runs out
Stop romanticizing your own impairment
Hannah Taylor
you know what i heard? the fda and big pharma made the sedating ones cheaper so people keep buying them. the safe ones are expensive on purpose. they want you to crash so you gotta buy more insurance and meds. its all a scheme. i only take the $4 benadryl now. they want you to think its dangerous but its just a conspiracy. i drive fine. i feel fine. they just dont want you to save money.
Peggy Adams
i dont even drive anymore. too many people on the road. and now this? i just stay home. honestly. why risk it. the world is rigged.
Sandy Crux
I find it profoundly amusing that you would presume to offer a 'simple action plan' to the masses-when the very premise of your argument relies on a reductive binary: 'safe' versus 'dangerous' antihistamines. Have you considered that individual metabolic variance, circadian rhythm, concurrent polypharmacy, and epigenetic expression may render your generalized recommendations not only insufficient but potentially hazardous to those with atypical pharmacodynamics? Furthermore, the assertion that fexofenadine is 'proven safe' is predicated on industry-funded trials with negligible sample diversity. I, for one, have experienced significant drowsiness on Allegra-while simultaneously exhibiting no impairment on cetirizine. Your moralizing tone is as unsubstantiated as your pharmacological absolutism.