Medication errors kill more people each year than car accidents. And a huge chunk of those errors happen when someone changes a dose - and no one catches it. It’s not always about bad intent. It’s often about rushed shifts, unclear handwriting, alert fatigue, or a simple miscommunication between providers. But here’s the truth: dose verification isn’t optional. It’s the last line of defense before a patient gets the wrong amount of a life-changing drug.
Why Dose Changes Are the Most Dangerous Moment
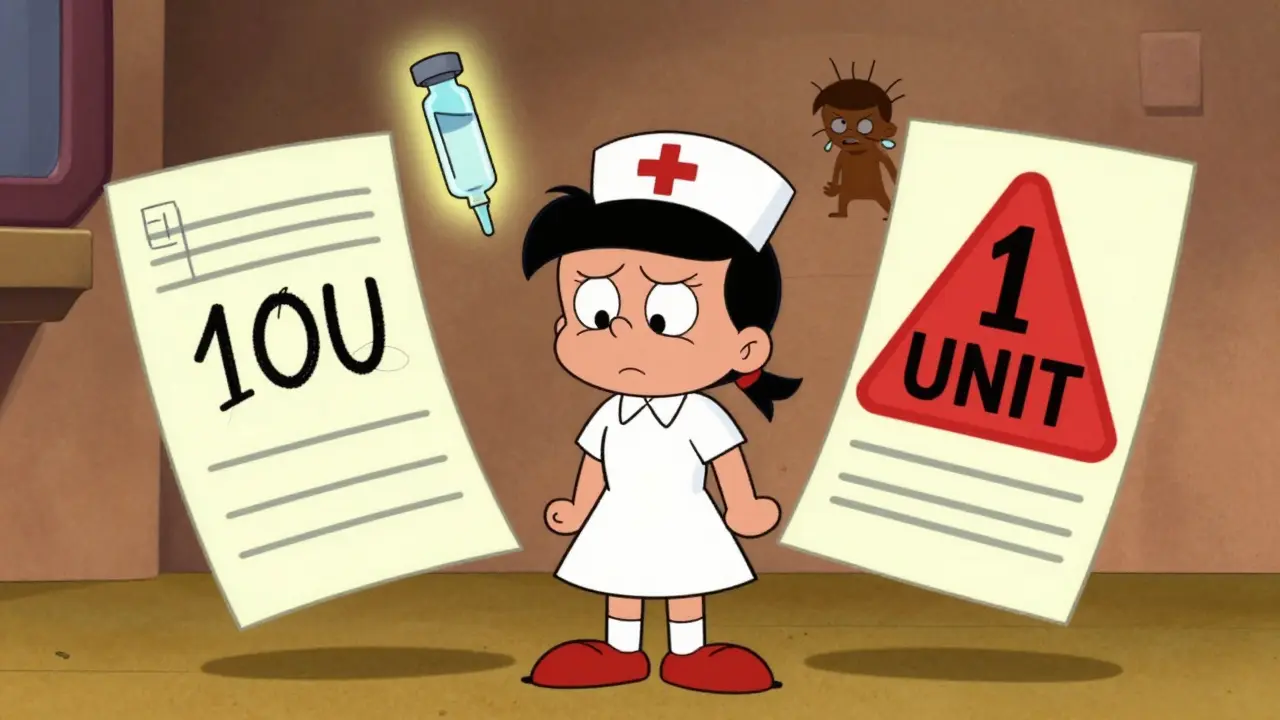
Changing a medication dose isn’t like adjusting the volume on a TV. One wrong digit - 10 units instead of 1 unit of insulin - can send a patient into a coma. Or worse. High-alert medications like heparin, opioids, insulin, and IV potassium are the usual suspects. But even common drugs like warfarin can turn deadly if the dose isn’t matched to the patient’s INR levels. The Joint Commission found that miscommunication during dose changes is the root cause of 65% of all medication-related sentinel events. That’s not a statistic. That’s someone’s parent, sibling, or child. The problem isn’t just the change itself. It’s how it’s passed along. A doctor scribbles “10U” on a paper chart. The nurse reads it as “10 units.” But the doctor meant “1.0 unit.” The double check happens - but both nurses assume the order is correct because it’s in writing. That’s not verification. That’s assumption.The Three-Step Verification Protocol That Works
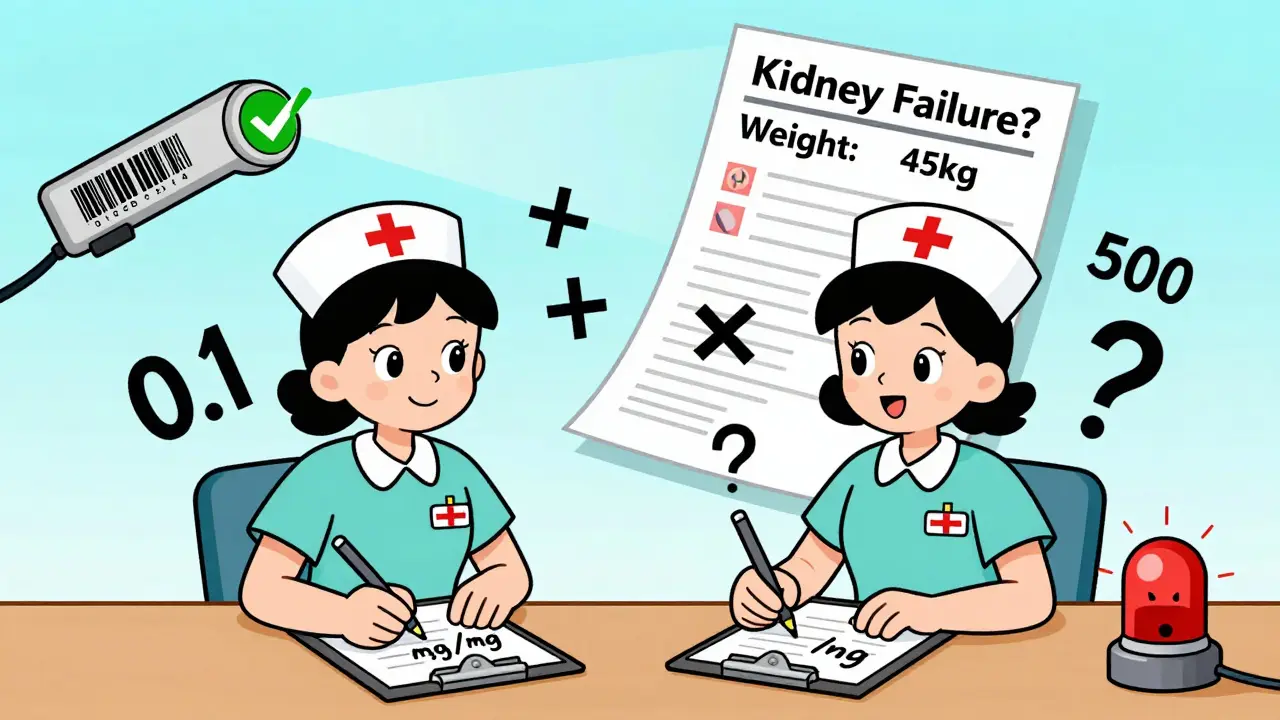
There’s no magic bullet. But there is a proven, step-by-step method used in top-performing hospitals. It’s called the 3-step verification, and it’s simple - if you actually do it.- Independent calculation - Two qualified providers do the math separately. No talking. No peeking. One calculates based on weight (0.1 mg/kg for pediatrics), renal function, or age. The other does the same. If they don’t match, stop. Investigate. This takes 2-3 minutes. Skip it, and you’re gambling with a life.
- Context check - Does this dose make sense for this patient? A 70-year-old with kidney failure doesn’t need the same dose as a 30-year-old athlete. Check labs. Check weight. Check allergies. Check recent changes in other meds. This step adds another 1-2 minutes. But skipping it? That’s how you give a warfarin dose to someone whose INR just dropped to 1.8 - and they bleed out two days later.
- Bedside barcode scan - Before you hand the drug to the patient, scan the patient’s wristband. Scan the medication. The system should confirm: right drug, right dose, right time, right route. If it flags a mismatch - even if you think it’s a glitch - pause. Call pharmacy. Recheck the order. This step takes 30-60 seconds. But it caught 86% of wrong-drug errors in one study. Don’t treat it like a nuisance alert. Treat it like your last safety net.
When Double Checks Help - And When They Don’t
You’ve heard it: “Always do a double check.” But that’s not the whole story. Independent double checks - where two people verify separately - are powerful. But only if you use them wisely. Studies show double checks catch 33% of dosing errors and up to 100% of wrong-vial errors in sepsis simulations. That’s huge. But here’s the catch: if you double-check everything, you start ignoring it. Nurses in one hospital reported skipping double checks during busy shifts because it felt like a ritual, not a safety step. And when you do that, you lose the benefit. The ISMP says it clearly: Don’t use double checks for everything. Use them only where the risk is highest. That means:- Insulin - always double check
- Heparin infusions - always double check
- Opioids in ICU - always double check
- Oral antibiotics? Maybe not. Unless the dose is unusual or the patient is high-risk.
Technology Isn’t the Hero - It’s the Helper
Barcode systems, smart pumps, and EHR alerts sound like the future. And they are. But they’re not perfect. Barcode scanning prevents 86% of wrong-drug, wrong-dose, and wrong-patient errors. But it can’t catch a dose that’s technically correct but clinically wrong. A pharmacist once told me: “Our system didn’t flag a 10-fold overdose because the concentration was entered right - just the dose was wrong.” Human eyes caught it. Because someone asked: “Why is this patient getting 500 mg of vancomycin? That’s not normal.” Smart infusion pumps with dose-error reduction software cut overdose errors by 85%. But they don’t know if the patient’s weight changed last night. Or if they’re now on dialysis. Or if they’re allergic to the dye in the IV bag. Technology is great at catching mistakes in the system. Humans are still the only ones who can catch mistakes in the thinking.Communication Is the Real Game-Changer
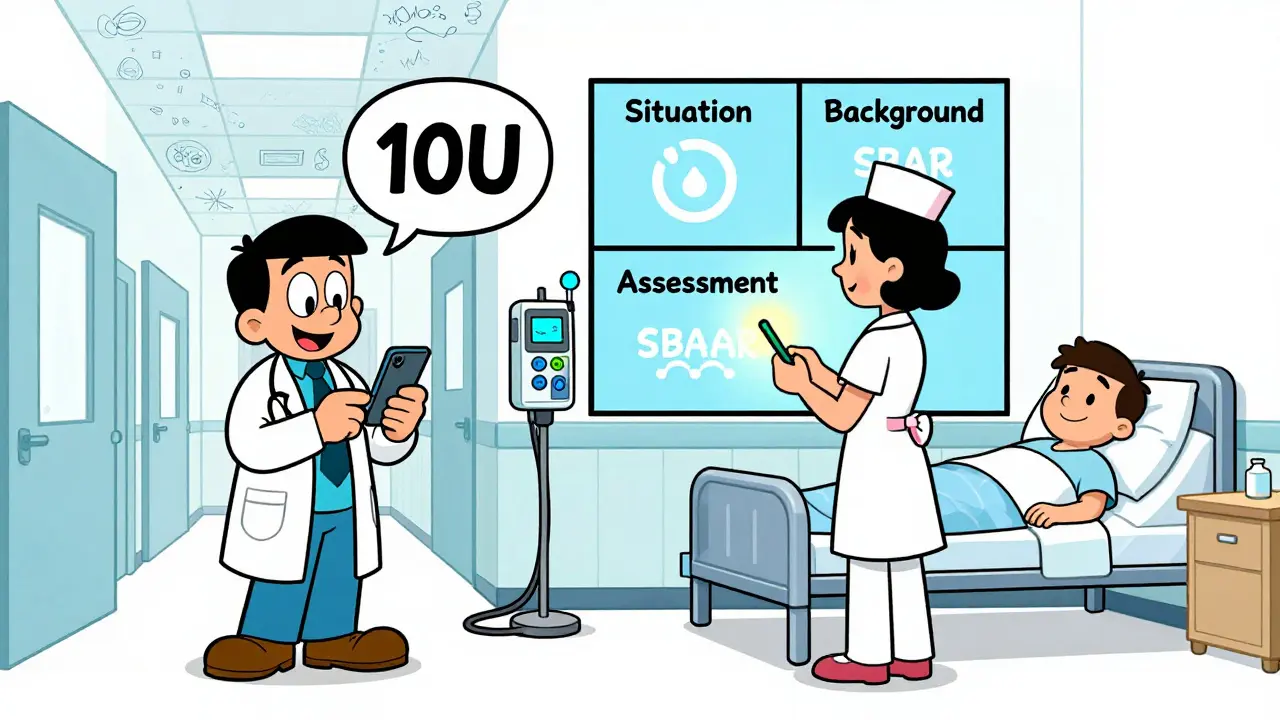
The biggest failure isn’t in the math. It’s in the handoff. When a patient moves from the ER to the floor, or from the ICU to a regular room, doses get changed. But who tells the nurse? A rushed phone call? A note in the chart? A text message? That’s where SBAR comes in. It’s not fancy. It’s just a structure:- Situation - “Patient X, 72, admitted for CHF, now on 20 mg furosemide daily.”
- Background - “Admitted with 8-pound weight gain, BNP 1200. Started on diuretic yesterday.”
- Assessment - “Today’s weight is down 4 pounds. No edema. Urine output 2L/day.”
- Recommendation - “I recommend reducing furosemide to 10 mg daily. Please verify with renal labs.”
What Happens When You Skip the Steps
In 2022, ECRI reported 1,247 incidents where dose changes weren’t verified properly. 287 of those caused patient harm. One nurse on Reddit shared: “I almost gave 10 units of insulin instead of 1 because the order said ‘10U’ and I didn’t question it. My partner caught it. We both broke out in a cold sweat.” Another nurse admitted: “I skipped the double check during my 12-hour shift because we were short-staffed. Two hours later, a patient went into hypoglycemia. Turned out the insulin dose was doubled.” These aren’t outliers. They’re symptoms of a broken system. When nurses are stretched too thin - nurse-to-patient ratios above 1:5 - verification adherence drops by 43%. That’s not negligence. That’s burnout.How to Make Verification Stick
You can’t fix this with posters or memos. You need structure.- Dedicate safety time - Johns Hopkins added 15-20 minutes per nurse shift just for verification. Errors dropped 37%.
- Train with simulations - Nurses who trained with mock dose errors had 89% adherence. Those who didn’t? 52%.
- Document everything - Time of verification, names of verifiers, lab values checked. Incomplete documentation caused 29% of verification failures.
- Use risk stratification - Don’t double-check every pill. Focus on high-alert meds, pediatric doses, and changes during transitions of care.
- Speak up without fear - If something feels wrong, say it. Even if the prescriber is the chief of medicine. Your voice is the last safety net.
The Bottom Line
Verification isn’t about following rules. It’s about protecting people. Every time you pause, calculate, scan, and confirm - you’re not just doing your job. You’re preventing a tragedy. The tools exist. The protocols are clear. The data is undeniable. What’s missing is consistency. Not because people don’t care. But because the system makes it hard to care the right way. Start small. Pick one high-alert medication. Implement the 3-step verification for it. Track your results. Share your wins. And then do it again for the next one. Because the next dose change? It could be your patient. And the next mistake? It might be yours.What’s the most common mistake in dose verification?
The most common mistake is assuming the order is correct because it’s written down. Handwritten orders with ambiguous abbreviations like “U” for units or “QD” for daily are major culprits. Even electronic orders can be wrong if the dose is entered correctly but the concentration is misconfigured. The fix? Always verify against the patient’s clinical context - weight, labs, renal function - not just the screen.
Do barcode systems really prevent errors?
Yes, but only if used correctly. Barcode medication administration (BCMA) prevents 86% of wrong-drug, wrong-dose, and wrong-patient errors when scanning compliance is above 95%. But if nurses bypass the system because it’s slow or glitchy, the protection vanishes. BCMA is strongest for matching drugs and patients - it can’t catch a dose that’s technically correct but clinically inappropriate.
When should you do an independent double check?
Only for high-alert medications: insulin, heparin, opioids, IV potassium, and chemotherapies. Also use it for pediatric doses, dose changes during care transitions, and when the dose is outside normal ranges. The ISMP warns against using double checks for everything - it leads to complacency. Focus on where the risk is highest.
Why do nurses skip verification steps?
Time pressure is the biggest reason. A 2022 American Nurses Association survey found 73% of nurses skipped steps during busy shifts. Other reasons include alert fatigue from too many system warnings, unclear protocols, and lack of support from leadership. When verification feels like an extra burden instead of a safety net, people cut corners.
What’s the role of SBAR in dose changes?
SBAR (Situation, Background, Assessment, Recommendation) is a communication tool that standardizes how dose changes are handed off between providers. Studies show it reduces miscommunication-related errors by 41%. It forces clarity: not just what the dose is, but why it’s being changed and what to watch for. It turns a rushed phone call into a structured safety check.
Are electronic systems replacing human verification?
No - and they shouldn’t. Systems like smart pumps and EHR alerts reduce specific errors, but they can’t replace clinical judgment. A machine won’t notice that a patient lost 10 pounds since yesterday or that their kidney function just dropped. Human verification is still essential to catch errors in context, not just in data.
How can hospitals improve verification compliance?
Start by reducing workload and increasing support. Add 15-20 minutes per shift for safety checks. Use simulation training - it boosts adherence to 89%. Eliminate unnecessary alerts. Make verification part of the workflow, not an add-on. And most importantly, create a culture where speaking up is rewarded, not punished.