What Are Immune-Related Adverse Events (irAEs)?
When cancer patients receive immune checkpoint inhibitors (ICIs), their immune system gets turned up to fight tumors. But sometimes, it doesn’t stop there. It starts attacking healthy organs too. These unintended side effects are called immune-related adverse events, or irAEs. They’re not like chemo side effects-nausea, hair loss, or fatigue. irAEs are autoimmune reactions. The body mistakes its own tissues for cancer cells. This can happen in the gut, skin, lungs, liver, thyroid, or even the heart and brain.
irAEs first became widely noticed after the FDA approved ipilimumab in 2011 for melanoma. Since then, they’ve been seen in nearly every type of cancer treated with ICIs. About 83% of people on CTLA-4 inhibitors, 72% on PD-1 blockers, and 60% on PD-L1 inhibitors will experience at least one irAE. Some show up within weeks. Others don’t appear until months after treatment ends. That’s why staying alert isn’t just for the first few months-it’s for as long as you’re on therapy, and sometimes even after.
Which Organs Are Most Affected?
Not all irAEs are the same. Some are common. Others are rare but deadly. The most frequent ones hit the gastrointestinal tract, skin, and endocrine system.
- Gut issues: Diarrhea, abdominal pain, and bloody stools are the top irAEs. Grade 3 or 4 colitis can be life-threatening if not caught early.
- Skin reactions: Rashes, itching, and blistering show up in over half of patients. Most are mild, but severe cases can look like toxic epidermal necrolysis.
- Thyroid problems: Hypothyroidism is common-fatigue, weight gain, cold intolerance. It’s often permanent and needs lifelong hormone replacement.
- Lung inflammation: Pneumonitis causes cough, shortness of breath, and low oxygen. It’s one of the deadliest irAEs, especially if missed.
- Liver damage: Elevated liver enzymes, jaundice, dark urine. Often found on routine blood tests before symptoms appear.
- Heart and brain: Myocarditis and neurotoxicity are rare, but they kill. A 2021 JAMA Oncology study found a 2.7% death rate among patients with cardiac irAEs.
Endocrine irAEs like hypophysitis or adrenal insufficiency need hormone replacement, not steroids. Giving steroids to someone with low cortisol won’t fix it-they need hydrocortisone or levothyroxine. Mistaking an endocrine issue for a general inflammation can delay treatment and put the patient at risk.
How Are irAEs Graded and Treated?
Doctors use the Common Terminology Criteria for Adverse Events (CTCAE) to grade severity. This isn’t just paperwork-it guides life-or-death decisions.
- Grade 1: Mild symptoms. No treatment needed. Just monitor.
- Grade 2: Moderate. Hold ICI therapy. Start oral prednisone at 1 mg/kg per day. Symptoms must drop to Grade 1 before restarting treatment.
- Grade 3: Severe. Stop ICI. Give IV methylprednisolone (1-2 mg/kg/day) for 3 days, then switch to high-dose oral prednisone. Specialist consult required within 24 hours.
- Grade 4: Life-threatening. ICU-level care. High-dose steroids, immediate specialist involvement, and often permanent discontinuation of immunotherapy.
Steroid tapering is critical. Too fast, and symptoms bounce back. Too slow, and side effects pile up. The standard is to reduce the dose over 4 to 6 weeks. Many patients struggle with this. Insomnia, weight gain, mood swings-steroids hit hard. One survey found 72% of patients had trouble sleeping, 65% gained weight, and 58% felt depressed or anxious during tapering.
What If Steroids Don’t Work?
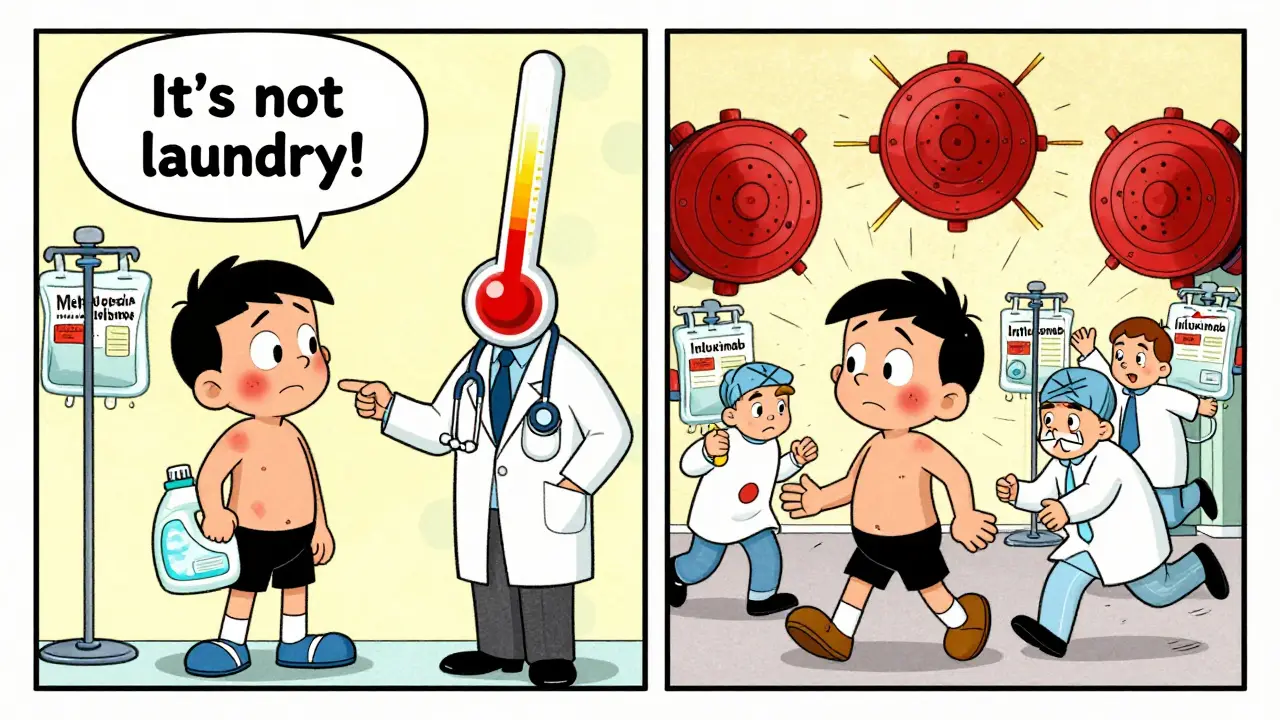
Not every patient responds to steroids. When symptoms don’t improve after 48 hours, it’s called steroid-refractory irAE. That’s when you move to second-line drugs.
- Infliximab: Blocks TNF-alpha. Used for colitis, pneumonitis, and some liver cases. Given as an IV infusion. Works fast-many patients improve in under a week.
- Mycophenolate mofetil: Used for liver or kidney irAEs. Slower than infliximab but good for long-term control.
- IVIG: Packed antibodies. Used for neurological or hematologic irAEs. Expensive, but effective when other drugs fail.
- Vedolizumab: Newer option. Targets gut-specific immune cells. A 2024 SITC guideline showed it worked in 68% of steroid-refractory colitis cases, better than infliximab’s 52%.
- Cyclophosphamide: Reserved for the toughest cases-like severe neurotoxicity or multi-organ failure.
Important: Treating irAEs doesn’t mean your cancer treatment fails. Multiple studies confirm that patients who get immunosuppressive therapy for irAEs still respond well to their cancer drugs. The fear that suppressing the immune system will let the tumor grow? That’s outdated.
Why Timing and Specialist Care Matter
irAEs don’t wait. Delayed treatment = worse outcomes. A 2023 Flatiron Health analysis showed that patients treated within 48 hours of symptom onset had hospitalization rates cut in half-from 34% to 19%.
But most community oncology clinics don’t have the tools or staff to handle this. A 2022 study found that hospitals with dedicated immune toxicity teams had 92% protocol adherence. Those without? Only 68%. That gap costs lives.
When a patient has Grade 3 or 4 irAE, you need specialists-fast. Gastroenterology for colitis. Endocrinology for thyroid or adrenal issues. Pulmonology for lung inflammation. Neurology for seizures or weakness. Oncology nurses report that 79% of patients don’t realize how urgent early symptoms are. A little diarrhea? They think it’s food poisoning. A rash? They blame laundry detergent. By the time they call, it’s Grade 3.
What’s New in irAE Management?
The field is moving fast. In 2024, the Society for Immunotherapy of Cancer updated its guidelines to include vedolizumab as a first-choice option for colitis that doesn’t respond to steroids. New real-world data from 12,500 patients shows that electronic health record alerts-like those now built into Epic Systems’ 2023 oncology module-help catch problems earlier.
Scientists are also looking for warning signs before symptoms appear. A 2023 Nature Medicine study found that patients with baseline IL-17 levels above 5.2 pg/mL had nearly five times the risk of severe irAEs. That could lead to blood tests before starting treatment to predict who’s at risk.
And patient education is finally getting attention. The European Society for Medical Oncology is rolling out standardized irAE guides in 15 languages. Right now, 41% of patients say they didn’t understand what symptoms to watch for. That’s unacceptable.
What Happens After Treatment?
Most irAEs resolve with treatment. About 85-90% of patients fully recover. But 10-15% end up with long-term issues. Hypothyroidism? Lifelong pills. Diabetes from pancreas damage? Daily insulin. Chronic colitis? Ongoing meds. Some patients need immunosuppressants for years.
That’s why follow-up doesn’t stop when the cancer treatment ends. Patients need regular blood work, endocrine checks, and symptom check-ins for months-even years. Many clinics now have irAE clinics run by nurse practitioners and pharmacists who specialize in this. They track steroid tapers, hormone levels, and patient-reported symptoms.
Final Thoughts: It’s Not Just About Cancer Anymore
irAEs aren’t a footnote in cancer care. They’re central to it. As more patients get immunotherapy-48% of U.S. cancer patients now qualify-doctors, nurses, and patients all need to know how to spot and respond to these side effects. The tools are here: guidelines, specialists, monitoring systems, new drugs. But success depends on one thing: acting fast, knowing the signs, and never assuming a symptom is "just something else."
Every rash, every bout of diarrhea, every new fatigue-these could be the body’s way of saying, "I’m fighting too hard." Listening to that signal can mean the difference between recovery and tragedy.
Can irAEs happen after stopping immunotherapy?
Yes. While most irAEs appear within the first 3 months of treatment, some show up weeks or even months after stopping immune checkpoint inhibitors. Cases of colitis, hepatitis, and neurotoxicity have been reported up to a year later. Patients must stay alert and report new symptoms-even if they think treatment is over.
Do steroids make cancer treatment less effective?
No. Early concerns suggested steroids might weaken the immune response against cancer, but multiple studies since 2020 have shown that using corticosteroids to treat irAEs does not reduce tumor response. Patients who receive steroids for irAEs have similar survival rates and cancer control as those who don’t.
Are there blood tests to predict irAEs before they happen?
Not yet standard, but promising research is underway. A 2023 study found that high baseline levels of IL-17 (above 5.2 pg/mL) strongly predict severe irAEs. Other biomarkers like specific T-cell patterns and gut microbiome changes are being studied. In the near future, blood tests may help identify high-risk patients before treatment even begins.
What should I do if I get a rash while on immunotherapy?
Don’t wait. Report it immediately to your oncology team. Mild rashes (Grade 1) may just need moisturizer and monitoring. But if it spreads, blisters, or is painful, it could be Grade 2 or higher. That means holding treatment and starting steroids. Delaying care can turn a manageable rash into a life-threatening skin condition.
Can I go back on immunotherapy after an irAE?
Sometimes. For Grade 1 or 2 irAEs that fully resolve, treatment may be restarted after steroid taper. For Grade 3 or 4, most guidelines recommend permanent discontinuation. But exceptions exist-especially if the cancer responded well and the irAE was mild and isolated. Decisions are made case-by-case with input from specialists.
Why do some patients need lifelong hormone replacement after irAEs?
Some irAEs permanently damage hormone-producing organs like the thyroid, pituitary, or adrenal glands. Once these glands are destroyed, they can’t recover. That means lifelong medication-like levothyroxine for hypothyroidism or hydrocortisone for adrenal insufficiency. These aren’t side effects of treatment-they’re the result of the immune system destroying tissue.