Beta-Blocker Hypoglycemia Risk Assessment Tool
Risk Assessment
When you're managing diabetes with insulin, even small changes in your medication can create hidden dangers. One of the most serious - and often overlooked - risks comes from combining insulin with beta-blockers. These heart medications, commonly prescribed for high blood pressure or after a heart attack, can quietly erase the warning signs of low blood sugar. For many people, this means a sudden collapse without any warning - no shaking, no racing heart, no sweat. And that’s not just scary. It’s life-threatening.
Why Your Body Stops Warning You
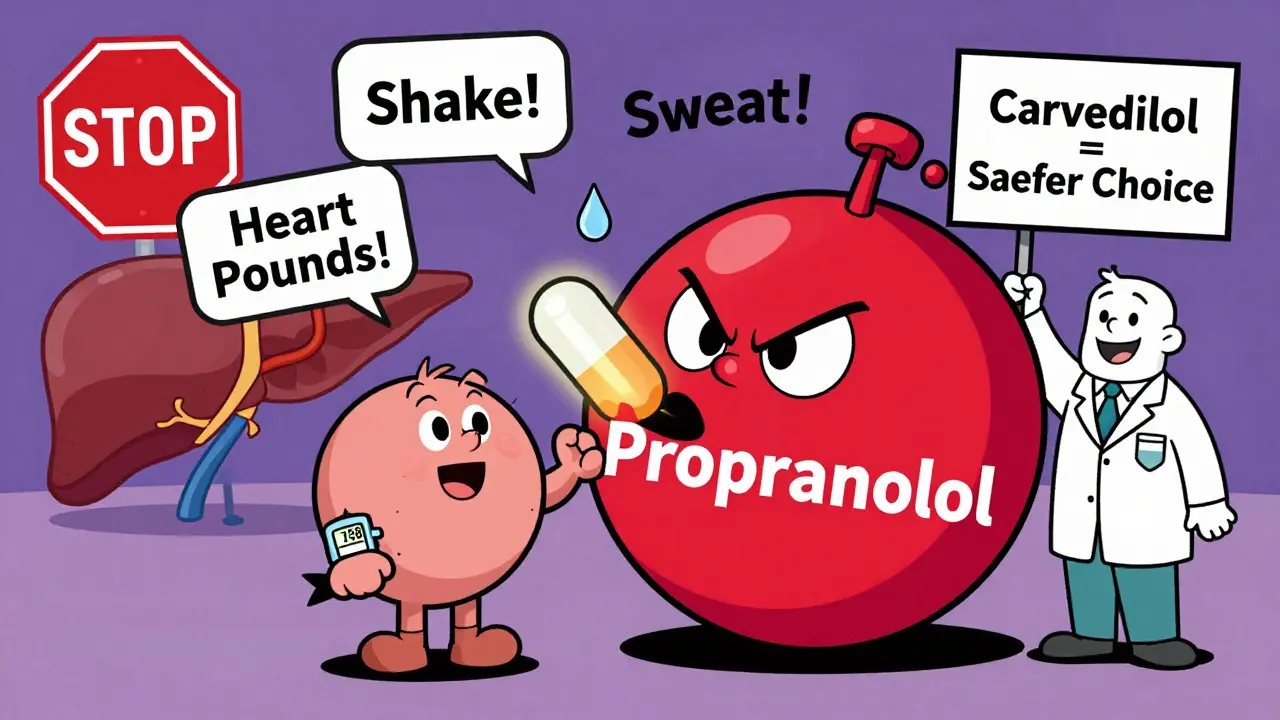
Hypoglycemia unawareness isn’t just a lack of symptoms. It’s your body’s alarm system going silent. Normally, when your blood sugar drops, your nervous system kicks in. You feel shaky, your heart pounds, your palms sweat. These are your body’s natural defenses - signals telling you to eat, to act, to survive. But beta-blockers change all that. They block the adrenaline response. That means the trembling and fast heartbeat - two of the strongest early warnings - vanish. You might not even notice your blood sugar is crashing until you’re confused, dizzy, or unconscious. This isn’t theoretical. Studies show that about 40% of people with type 1 diabetes develop this unawareness over time, and beta-blockers make it far worse.The Hidden Mechanism: More Than Just Masking Symptoms
Many assume beta-blockers only hide symptoms. That’s half the story. The real danger is that they also stop your body from fixing the problem. When your blood sugar drops, your liver should release stored glucose to bring it back up. Beta-blockers - especially the selective ones like atenolol or metoprolol - directly block this process. They interfere with glycogen breakdown in your liver and muscles. So now you’ve got no warning and no backup. Worse, some beta-blockers also reduce insulin clearance, meaning insulin stays active longer in your body. This increases the chance of a prolonged, deep low. It’s a double hit: your body can’t tell you’re in trouble, and it can’t fix it either.Not All Beta-Blockers Are the Same
This is where things get critical. Not every beta-blocker carries the same risk. The difference between drug types isn’t just academic - it’s the difference between safety and crisis.- Non-selective beta-blockers (like propranolol) block both heart and lung receptors. These are the worst offenders. They wipe out nearly all adrenaline symptoms and carry the highest risk of severe hypoglycemia.
- Selective beta-blockers (like metoprolol, atenolol) mainly target the heart. They still mask symptoms, but less completely. Still, research shows they increase the odds of hypoglycemia by 2.3 times in hospitalized patients.
- Carvedilol is different. It’s not just a beta-blocker - it also blocks alpha receptors. This gives it a unique advantage. Studies show carvedilol causes far less disruption to glucose recovery. In fact, one study found patients on carvedilol had a 17% lower risk of severe hypoglycemia compared to those on metoprolol. For people on insulin, this makes carvedilol the safer choice.
One Warning Sign Still Works - And You Need to Know It
Here’s the one thing you can still count on: sweating. Unlike trembling or a racing heart, sweating isn’t triggered by adrenaline. It’s controlled by acetylcholine, a different chemical pathway. That means even if you’re on a beta-blocker, you’ll still sweat when your blood sugar drops. This is huge. If you’re on insulin and a beta-blocker, your new warning signal is sweat. Not shakiness. Not palpitations. Sweating. If you suddenly feel clammy, damp, or cold - even if you’re not hot or stressed - check your blood sugar. Immediately.
Who’s at Highest Risk?
Not everyone on insulin and beta-blockers will have a problem - but some groups are in serious danger:- People with type 1 diabetes - especially those with a history of low blood sugar
- Patients recently started on beta-blockers - 68% of dangerous lows happen in the first 24 hours
- Those with kidney disease - insulin clears slower, making lows more likely
- People who don’t check their blood sugar regularly
- Anyone using long-acting insulin without a backup plan
What Hospitals Are Doing - And What You Should Do Too
Hospitals have learned the hard way. The American Diabetes Association now recommends blood glucose checks every 2 to 4 hours for diabetic patients on beta-blockers. Why? Because lows can spike fast - and silently. At home, you need the same vigilance:- Check your blood sugar before meals, before bed, and anytime you feel “off” - even if you don’t feel the classic symptoms
- Set alarms on your phone or CGM to check every 4 hours overnight if you’re at risk
- Always carry fast-acting glucose (glucose tabs, juice, or gel) - not candy
- Teach family or roommates to recognize sweating as a warning sign
- Never skip meals or delay eating if you’ve taken insulin
Technology Is Your Lifeline
Continuous glucose monitors (CGMs) have changed the game. Since 2018, use of CGMs in people on insulin and beta-blockers has jumped 300%. Why? Because they don’t rely on your body’s signals. They give you real-time numbers - and alarms - even while you sleep. Studies show CGMs reduce severe hypoglycemia by 42% in this high-risk group. If you’re on insulin and a beta-blocker, and you don’t have a CGM, you’re flying blind. Talk to your doctor. Insurance usually covers it if you’re on insulin and have a history of lows.
The Bigger Picture: Heart vs. Blood Sugar
This is the toughest part. Beta-blockers save lives. After a heart attack, they cut the risk of death by 25%. For people with diabetes - who already have a much higher risk of heart disease - that benefit is huge. But here’s the truth: you don’t have to choose between heart health and blood sugar safety. You can have both - if you’re smart about it.- Switch to carvedilol if you’re on a higher-risk beta-blocker
- Use a CGM
- Check your numbers more often
- Never stop a beta-blocker without talking to your doctor
What to Ask Your Doctor
If you’re on insulin and a beta-blocker, here are the five questions you need to ask:- Is this beta-blocker the best choice for me, given my diabetes?
- Could I switch to carvedilol to lower my hypoglycemia risk?
- Am I a candidate for a continuous glucose monitor?
- What should I do if I start sweating without an obvious reason?
- Do I need to change my insulin dose now that I’m on this medication?
The Bottom Line
Combining insulin and beta-blockers doesn’t mean you have to live in fear. But it does mean you need to be smarter. The symptoms you used to rely on? They’re gone. Your body’s natural safety net? It’s disabled. That leaves you with one job: take control. Check your numbers. Use your monitor. Know your sweat. Choose the right drug. Talk to your care team. This isn’t about avoiding medication. It’s about using it safely. Because the goal isn’t just to live longer - it’s to live without surprises. And with the right steps, you can.Can beta-blockers cause low blood sugar on their own?
Beta-blockers don’t directly cause low blood sugar, but they make it more likely and more dangerous when it happens. They interfere with the body’s ability to recover from low glucose by blocking the liver’s release of stored sugar. When combined with insulin, this increases the risk of severe, prolonged lows.
Why is sweating the only reliable warning sign?
Sweating during low blood sugar is triggered by acetylcholine, not adrenaline. Beta-blockers block adrenaline responses - which stop trembling and fast heartbeat - but they don’t affect acetylcholine. That means sweating remains intact. If you suddenly feel damp or cold without exertion or heat, check your blood sugar immediately.
Is carvedilol really safer than other beta-blockers?
Yes. Carvedilol blocks both beta and alpha receptors, which helps preserve the body’s ability to recover from low blood sugar. Studies show it’s associated with a 17% lower risk of severe hypoglycemia compared to metoprolol. For people on insulin, it’s often the preferred choice when a beta-blocker is needed.
Do I need to stop my beta-blocker if I have hypoglycemia unawareness?
No - not unless your doctor recommends it. Stopping beta-blockers can be dangerous, especially if you have heart disease. Instead, focus on reducing risk: switch to carvedilol, use a CGM, check your blood sugar more often, and learn to recognize sweating as your new warning sign.
Can I still drive if I’m on insulin and a beta-blocker?
Yes - but with strict precautions. Always check your blood sugar before driving. Keep glucose tabs in the car. Use a CGM with alerts. Avoid long drives without stopping. If you’ve had a recent low or don’t feel symptoms, don’t drive until you’re confident your body is responding normally.
For those managing both diabetes and heart disease, the path forward isn’t about giving up one medication for another. It’s about working smarter - using the right tools, knowing the signs, and making informed choices. Because when you understand the risks, you’re not at their mercy. You’re in control.