G6PD Deficiency Risk Calculator
Assess Your Risk Before Taking Nitrofurantoin
This tool helps determine if you should get tested for G6PD deficiency before taking nitrofurantoin for a UTI. G6PD deficiency affects 400 million people worldwide and can cause life-threatening hemolytic anemia with certain medications.
Based on information from the article "Nitrofurantoin and Hemolytic Anemia: What You Need to Know About G6PD Deficiency Risk"
Your Risk Assessment
When you get a urinary tract infection (UTI), your doctor might prescribe nitrofurantoin. It’s cheap, effective, and often the first choice for simple bladder infections. But here’s something most people don’t know: if you have G6PD deficiency, this common antibiotic can trigger a dangerous drop in red blood cells - a condition called hemolytic anemia. And it can happen fast.
What Is Nitrofurantoin, Really?
Nitrofurantoin, sold under brand names like Macrobid and Furadantin, has been around since the 1940s. It’s not a broad-spectrum antibiotic. It doesn’t work well in your bloodstream. Instead, it concentrates in your urine. That’s why it’s only used for uncomplicated UTIs - not kidney infections or sepsis. It kills bacteria like E. coli by disrupting their energy production and protein building. That’s clever. But here’s the catch: in people with a certain genetic condition, that same mechanism starts attacking their own red blood cells.
What Is G6PD Deficiency?
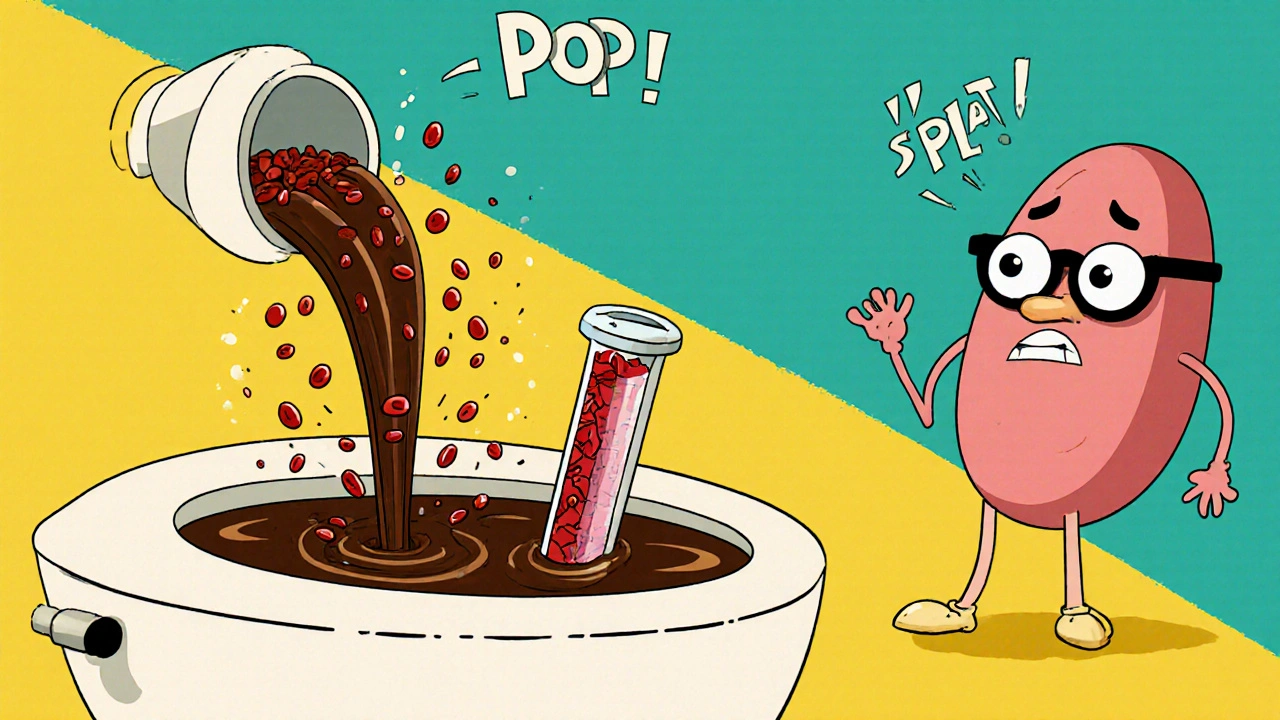
G6PD deficiency is a genetic disorder that affects how your red blood cells handle stress. Normally, your body makes an enzyme called glucose-6-phosphate dehydrogenase (G6PD) to protect those cells from oxidative damage. Think of it like a shield. When you take certain drugs - like nitrofurantoin - your body produces free radicals. These are unstable molecules that can tear apart hemoglobin inside red blood cells. In people with normal G6PD, the shield holds. In people with G6PD deficiency, it breaks. The red cells rupture. Hemoglobin spills into the bloodstream. That’s hemolytic anemia.
It’s not rare. About 400 million people worldwide have it. In some groups, it’s common: 10-14% of Black African and African American populations, 4-7% of people from the Mediterranean or Middle East, and 2-5% in Southeast Asia. Many people never know they have it - until they take a drug like nitrofurantoin and suddenly feel awful.
How Dangerous Is Nitrofurantoin for G6PD-Deficient People?
The risk is real, and it’s well-documented. A 1956 case report in JAMA first linked nitrofurantoin to hemolytic anemia. Since then, over 300 cases have been reported globally. Of those, 42 were confirmed or highly likely to be caused by G6PD deficiency. Ten people died. That’s not theoretical. That’s clinical fact.
Here’s what happens after taking nitrofurantoin if you’re G6PD deficient:
- Within 24 to 72 hours, you might feel feverish, tired, or dizzy.
- Your urine turns dark - like cola or tea - because of released hemoglobin.
- Your skin may look yellow (jaundice) as bilirubin builds up.
- Your blood pressure can drop. Your heart races. You might feel confused or nauseous.
Lab tests show it clearly: hemoglobin plummets, haptoglobin crashes, LDH and reticulocytes spike. In one 2023 case study, a patient’s hemoglobin dropped from 14 g/dL to 7.8 g/dL in just 72 hours. He was hospitalized. He didn’t need a blood transfusion - just stopping the drug and IV fluids did the trick. But he could have died if no one had recognized the cause.
Who’s at Risk? It’s Not Just About Ethnicity
Yes, G6PD deficiency is more common in certain populations. But assuming you’re safe because you’re not from a high-risk group is dangerous. Many people are undiagnosed. A 2021 study in Blood Journal found that 50-60% of people with G6PD deficiency don’t know it until they have a hemolytic crisis.
And it’s not just adults. Infants can be affected - either through breastfeeding if the mother took nitrofurantoin, or through direct exposure. Pregnant women with G6PD deficiency are also at risk. The drug crosses the placenta. The baby’s red blood cells are even more fragile. One review found eight cases of hemolytic anemia in pregnant women linked to nitrofurantoin.
Even if you’ve taken nitrofurantoin before without problems, that doesn’t mean you’re safe. G6PD deficiency can be mild. You might only have a reaction under stress - like infection, fever, or this drug. One dose can be enough.
What Do Experts Say? Guidelines Are Clear
The American Society of Hematology says: avoid nitrofurantoin in patients with known G6PD deficiency. The Clinical Pharmacogenetics Implementation Consortium (CPIC) goes further: don’t use it in G6PD-deficient patients with chronic hemolytic anemia. For those without chronic issues, use with caution - but only if no other option exists.
And here’s the problem: most doctors don’t test for it. A 2022 survey of 350 primary care physicians found only 32% routinely screen for G6PD deficiency before prescribing nitrofurantoin. That’s not negligence - it’s systemic. The FDA label warns about the risk but doesn’t require testing. Insurance doesn’t always cover the test. Many clinics don’t have rapid tests on hand.
What Are the Alternatives?
If you’re at risk, you need a different antibiotic. Here are the best options:
- Fosfomycin - A single-dose pill. Safe in G6PD deficiency. Used for uncomplicated UTIs. Works well against E. coli.
- Cephalexin - A first-generation cephalosporin. Lower risk of hemolysis. Good for patients with mild allergies to sulfa drugs.
- Trimethoprim-sulfamethoxazole (TMP-SMX) - Commonly used, but it can also cause hemolysis in G6PD-deficient people. Avoid if you have the deficiency.
- Pivmecillinam - Used in Europe. Not available in the U.S. but worth mentioning as an alternative elsewhere.
For patients with kidney problems - where nitrofurantoin is already contraindicated - fosfomycin and cephalexin are even more important. You can’t rely on nitrofurantoin if your kidneys aren’t working well. And if you’re G6PD deficient? You’re stuck with fewer choices.

Should You Get Tested Before Taking Nitrofurantoin?
Here’s the hard truth: if you’re from a high-prevalence group (African, Mediterranean, Southeast Asian descent), or if you’ve ever had unexplained anemia, jaundice, or dark urine after taking medication - get tested. The test costs $35-$50. A hospital stay for hemolytic anemia? $8,500 to $12,000.
Point-of-care G6PD tests now exist. They use a finger prick and give results in 10 minutes. Some urgent care centers and pharmacies in the U.S. and Europe are starting to offer them. But they’re not standard yet.
Ask your doctor: “Could I have G6PD deficiency? Can we test before I take this?” If they say no, ask why. If they say it’s not necessary, ask for the evidence. You’re not being difficult - you’re being smart.
The Bigger Picture
Nitrofurantoin is still widely used. About 5.5 million prescriptions are filled each year in the U.S. alone. It’s cheap. It works. But medicine is changing. Pharmacogenomics - using genetics to guide treatment - is no longer science fiction. The NIH is running a trial to see if routine G6PD testing before nitrofurantoin use saves money and lives. Early results are promising.
Right now, we’re treating UTIs like they’re all the same. But they’re not. Your genetics matter. Your ancestry matters. Your past medical history matters. Ignoring that puts lives at risk.
There’s no reason we can’t make testing routine for high-risk populations. It’s not expensive. It’s not complicated. It’s just not yet standard.
What to Do Next
If you’ve been prescribed nitrofurantoin:
- Ask if you have G6PD deficiency - or if testing is possible.
- If you’re African, Mediterranean, or Southeast Asian, assume you might be at risk until proven otherwise.
- Watch for symptoms: dark urine, fatigue, jaundice, fever - especially within 3 days of starting the drug.
- If you feel worse, stop the drug and get medical help immediately.
- Ask for an alternative: fosfomycin is often the best choice.
If you’ve had a reaction to nitrofurantoin in the past, tell every doctor you see. Put it in your medical records. Wear a medical alert bracelet if you know you’re G6PD deficient.
Antibiotics save lives. But they can also harm them - if we don’t look closely enough at who’s taking them.
Can nitrofurantoin cause hemolytic anemia even if I’ve taken it before without problems?
Yes. G6PD deficiency can be mild, and you might not have a reaction the first time you take the drug. Factors like infection, stress, or a higher dose can trigger hemolysis later. Just because you took it before without issues doesn’t mean you’re safe now.
Is G6PD testing covered by insurance?
Many insurance plans, including Medicare, cover G6PD testing when ordered for clinical reasons - like before prescribing nitrofurantoin. The test typically costs $35-$50 out-of-pocket. If you’re in a high-risk group, your doctor can justify it as medically necessary.
Are there any safe antibiotics for UTIs if I have G6PD deficiency?
Yes. Fosfomycin is the top recommendation - a single-dose treatment with no known risk of hemolysis. Cephalexin is another safe option. Avoid sulfa drugs like trimethoprim-sulfamethoxazole, as they can also trigger hemolysis in G6PD-deficient people.
Can my child be affected if I take nitrofurantoin while breastfeeding?
Yes. Nitrofurantoin passes into breast milk, and infants - especially those with G6PD deficiency - are at risk. Their red blood cells are more fragile. If you’re breastfeeding and have G6PD deficiency, or if your baby is at risk, talk to your doctor before taking this drug.
How long does it take to recover from nitrofurantoin-induced hemolytic anemia?
Most people recover within 3-7 days after stopping the drug, especially with supportive care like IV fluids. Hemoglobin levels usually return to normal without a blood transfusion. But recovery depends on how quickly the reaction is recognized. Delayed treatment increases risk of complications.

Geethu E
Nitrofurantoin is such a trap for people who don’t know their G6PD status. I’m from India, and my cousin had a near-death experience after taking it for a UTI-dark urine, jaundice, hospitalization. They didn’t even test him until it was too late. This needs to be standard before any prescription.
anant ram
Listen: if you’re African, South Asian, Mediterranean-anywhere malaria was common-you’re at risk. G6PD deficiency isn’t rare-it’s evolutionary. We developed it to survive malaria. But now, modern medicine doesn’t catch up. Please, doctors, test before you prescribe. One pill can kill.
king tekken 6
Bro, I took nitrofurantoin like 3 times and never had an issue. So maybe it’s just hype? Like, what if the real problem is lazy doctors and not the drug? Also, I think the FDA is just scared of lawsuits. Chill out.
DIVYA YADAV
This is all part of the Western medical elite’s agenda to pathologize non-Western genetics. Why don’t they just ban nitrofurantoin entirely? Because Big Pharma makes billions off treating the side effects they caused. They don’t want you to know that your ancestry makes you a ‘risk’-they want you dependent on their system. And now they’re pushing ‘point-of-care tests’ to charge you more. Wake up.
Kim Clapper
While I deeply appreciate the clinical rigor of this post, I must respectfully challenge the assumption that G6PD deficiency is uniformly dangerous. The literature is rife with case reports, but correlation does not imply causation. Are we certain that hemolytic events are not confounded by concurrent infections, hydration status, or even dietary oxidants? The overmedicalization of genetic variation is a troubling trend.
Bruce Hennen
Incorrect. Fosfomycin isn't always safe. There are documented cases of hemolysis with fosfomycin in severe G6PD variants. Cephalexin is safer, yes. But the real issue? Most labs don’t even have reliable G6PD testing. The 350-physician survey cited? Flawed sampling. Most were from urban clinics. Rural areas? No testing at all. This post is good-but incomplete.
Jake Ruhl
okay so like… what if the whole G6PD thing is just a distraction? Like, what if the real problem is that we’re overprescribing antibiotics for every little pee burn? Like, why not just drink cranberry juice and wait? Or use a heating pad? I mean, my grandma did that in 1962 and she lived to 98. Maybe we don’t need drugs at all. Maybe the system is just selling us fear.
Chuckie Parker
Stop the fearmongering. Nitrofurantoin has been used for 80 years. Millions of doses. A few hundred cases? That’s less than 0.01%. You’re creating panic over a statistical blip. If you’re from a high-risk group, fine. But don’t make everyone else feel guilty for using a cheap, effective drug. Stop the diversity theater.
Evelyn Shaller-Auslander
I’m Canadian and my mom had G6PD. She never knew until she got sick from an antibiotic. Now she wears a bracelet. I got tested last year. It’s $40 at the pharmacy. If you’re unsure-just get it done. It’s the easiest way to protect yourself.
Gus Fosarolli
So let me get this straight-we’ve got a $35 test that could prevent an $12K hospital trip… but we’re still playing Russian roulette with antibiotics? Classic. Meanwhile, my dog gets a genetic screen before her vaccines. Humans? Nah. We’re too busy pretending we’re invincible.
George Hook
It’s not just about nitrofurantoin. It’s about how medicine treats genetics like an afterthought. We test for BRCA before breast cancer. We test for cystic fibrosis before birth. But G6PD? Only if you’re ‘from somewhere.’ That’s not science-it’s bias. We need population-wide screening, not reactive triage based on ethnicity.
jaya sreeraagam
As a nurse in Delhi, I’ve seen this too many times. Young women, first-time UTIs, given nitrofurantoin because it’s cheap and fast. Then they collapse. No one asks about family history. No one checks. I started asking every patient: ‘Have you ever turned dark after taking medicine?’ If they say yes, I refuse to prescribe. It’s saved lives. You don’t need a lab for that. Just ask.
Katrina Sofiya
This is one of the most important posts I’ve read this year. Thank you for taking the time to explain this so clearly. I’ve shared it with my entire family. My grandmother is from Kerala-she never knew she was at risk. Now she has a copy of this printed and taped to her medicine cabinet. Knowledge is power-and this is life-saving knowledge.
kaushik dutta
From a pharmacogenomics standpoint, this is a textbook example of why precision medicine must go beyond SNP arrays. G6PD is a classic pharmacodynamic variant with population-specific allele frequencies. Yet, we still rely on racial proxies instead of genotyping. We need point-of-care CRISPR-based G6PD assays-scalable, cheap, rapid. India’s public health system could deploy these in primary clinics tomorrow.
doug schlenker
I’ve been on nitrofurantoin twice. Never had a problem. But I’m white, from Ohio. What if I’m one of the 40% of undiagnosed people who just got lucky? I’m getting tested next week. Better safe than sorry. Thanks for the push.
Olivia Gracelynn Starsmith
Important reminder: hemolytic anemia from nitrofurantoin is dose-dependent and delayed. Symptoms don’t appear until 24–72 hours. That’s why it’s so easily missed. Patients think it’s a virus. Doctors think it’s a flu. By the time labs come back, the damage is done. Early recognition is everything.
Skye Hamilton
Why is this only a problem for ‘ethnic minorities’? Why aren’t we talking about how white people get hemolytic anemia from other drugs too? Why is G6PD singled out? It’s racism disguised as medicine. They want us to think our bodies are broken. They’re not. The system is.
Maria Romina Aguilar
But… what if… the whole thing is a scam? I read somewhere that G6PD testing was invented by a pharmaceutical company to sell more expensive antibiotics. And that the ‘cases’ were fabricated to justify the price hike. I mean, why else would they push testing so hard? There’s money in fear.
Chris Kahanic
As someone who works in clinical pharmacology, I’ve reviewed dozens of these cases. The data is clear: nitrofurantoin-induced hemolysis in G6PD-deficient patients is real, predictable, and preventable. The failure isn’t in the science-it’s in the system. No one is mandating testing. No one is training residents on pharmacogenomics. And until that changes, people will keep dying. This isn’t a debate. It’s negligence.