Steroid Myopathy Risk Assessment Tool
Risk Assessment
This tool calculates your risk of steroid myopathy based on your steroid dosage and duration.
Timed Chair Rise Test
Time how long it takes to stand up from a chair five times without using your arms. Normal is under 10 seconds.
Important: This tool is for informational purposes only. Always consult your healthcare provider for medical diagnosis and treatment recommendations.
When you’re on long-term steroids for asthma, rheumatoid arthritis, or another chronic condition, you expect relief - not new problems. But for many, a quiet, painless weakness creeps in. You can’t stand up from a chair without using your arms. Climbing stairs feels impossible. Lifting your arms to reach a shelf becomes a struggle. And there’s no pain. No swelling. No red flags. Just slow, steady loss of strength. This isn’t just being out of shape. It’s steroid myopathy.
What Exactly Is Steroid Myopathy?
Steroid myopathy is muscle weakness caused by taking corticosteroids like prednisone, dexamethasone, or cortisone for more than a few weeks. It’s not an infection. It’s not inflammation. It’s a direct toxic effect on your muscle fibers. First noticed in the 1930s in patients with Cushing’s syndrome, it’s now one of the most common drug-related muscle problems worldwide. Up to 21% of people on chronic steroid therapy develop it, and in critical care settings, it can show up in just two to three weeks with high doses. The real kicker? It’s often missed. Doctors assume weakness is from the original illness - like COPD or lupus - or just from being bedridden. But studies show nearly 40% of cases are misdiagnosed. That’s why so many people suffer for months before anyone connects the dots.How Do You Know It’s Steroid Myopathy - Not Something Else?
The weakness is specific. It hits the muscles closest to your body’s center - the hips, thighs, and shoulders. The legs usually go first. You’ll struggle to rise from a chair, climb stairs, or lift your arms overhead. But here’s the thing: there’s no pain. No cramps. No burning. That’s a big clue. Inflammatory muscle diseases like polymyositis hurt. Steroid myopathy doesn’t. Blood tests don’t help much either. Creatine kinase (CK), a marker of muscle damage, stays normal - usually between 30 and 170 U/L. In other muscle diseases, CK shoots up over 500. Electromyography (EMG) looks normal too. No signs of nerve damage or inflammation. Muscle biopsies show something more telling: type 2b muscle fibers shrink. These are the fast-twitch fibers you use to stand up quickly, climb stairs, or lift heavy things. They’re the first to go under steroid stress. And unlike inflammatory myopathies, steroid myopathy doesn’t get worse when you stop the steroids. In fact, it often improves - slowly - once the dose is lowered or stopped. That’s a key difference.Who’s at Risk?
Anyone on long-term steroids is at risk. But some groups are more vulnerable:- People taking more than 10 mg of prednisone daily for four weeks or longer
- Patients on high-dose IV steroids in ICUs (40-60 mg daily)
- Those using dexamethasone - it’s more likely to cause weakness than prednisone
- Older adults, especially over 65
- People with diabetes or poor nutrition
Why Does This Happen?
Steroids don’t just fight inflammation - they mess with how your muscles build and break down protein. They turn on enzymes that tear down muscle fibers (ubiquitin-proteasome system) and turn off signals that build new ones. Think of it like a factory where the assembly line shuts down while the trash compactor runs full speed. Muscle fibers shrink. Strength drops. And because type 2b fibers are the most energy-hungry, they’re the first to be broken down. It’s not just about dose and time. Genetics, age, and other medications play a role too. Some people can take 20 mg of prednisone for years with no issues. Others notice weakness at 5 mg. There’s no clear predictor - which is why screening matters.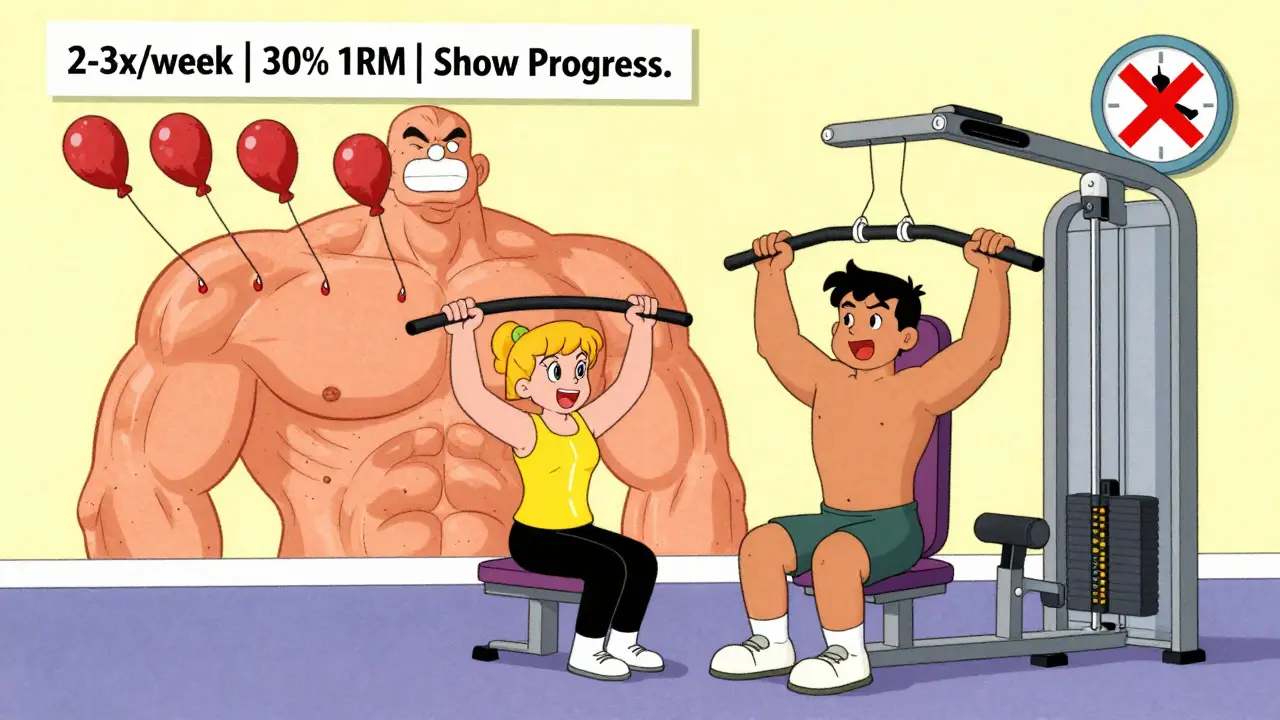
How Is It Diagnosed?
There’s no single blood test. Diagnosis comes from recognizing the pattern: chronic steroid use + painless proximal weakness + normal CK + normal EMG. Doctors can use simple functional tests to catch it early:- Timed Chair Rise Test: Time how long it takes to stand up from a chair five times without using your arms. Normal is under 10 seconds. People with steroid myopathy often take 15-25 seconds.
- Gower’s Maneuver: Can you get up from the floor without using your hands? If you have to push with your arms, crawl up your legs, or use furniture, that’s a red flag.
- Shoulder Abduction Test: Can you lift your arms sideways to shoulder height? Weakness here is common but often overlooked.
Physical Therapy: The Only Proven Treatment
The good news? You can reverse this. Physical therapy isn’t just helpful - it’s essential. The goal isn’t to build bulk. It’s to rebuild the fast-twitch fibers that steroids destroyed. That means resistance training - but not too hard. High-intensity workouts can make things worse by increasing muscle breakdown. The American Physical Therapy Association recommends:- 2-3 sessions per week of moderate resistance training
- Starting at 30% of your one-rep max (the most weight you can lift once)
- Progressing slowly - only 5-10% more weight every two weeks
- Focusing on leg presses, squats, step-ups, and seated shoulder presses
What About Stopping Steroids?
You can’t just quit steroids. For many, they’re life-saving. Stopping them suddenly can trigger adrenal crisis. The key is to reduce the dose slowly - under medical supervision - while starting physical therapy. Even if you can’t reduce your dose, exercise still helps. One patient on 15 mg of prednisone daily for lupus improved her ability to climb stairs by 40% in three months with consistent training - even though her steroid dose didn’t change.What Doesn’t Work
Don’t waste time on these:- Stretching alone - doesn’t rebuild muscle
- Cardio-only programs - walking helps circulation, but won’t restore strength
- High-intensity weightlifting - can cause more damage
- Supplements like creatine or protein shakes - no solid evidence they help in steroid myopathy

Ron Williams
Been on prednisone for lupus for 8 years. Thought I was just getting old. Turns out I’ve been doing chair rises with my arms like a confused penguin. This post? Lifesaver. Started PT last week. Already feel less like a rusty robot.
James Rayner
It’s wild… we treat inflammation like the enemy… but our muscles? They’re just trying to survive the chemical war we’re waging inside them. 🤔💊
Maybe the real question isn’t ‘how do we fix the weakness?’… but ‘why did we think this was a fair trade?’
Dave Alponvyr
So… you’re telling me the thing keeping me alive is slowly turning me into a human who can’t get off the couch? Cool. Thanks, Big Pharma.
Cassandra Collins
They don’t want you to know this. Steroids are a gateway. Next thing you know, they’re putting chips in your muscles to track your weakness. The CDC knows. They just won’t tell you. 😈
Joanna Ebizie
Ugh. Of course it’s not painful. Pain is for people who actually care about their bodies. You people take steroids like candy and then act shocked when you turn into jelly.
Elizabeth Bauman
This is why we need to stop letting foreign doctors prescribe this stuff. In America, we used to fix problems with hard work and discipline. Now we just get weak and blame the medicine. Pathetic.
Dylan Smith
I’ve been doing leg presses at 30% and it’s actually working… I didn’t think it would
My PT said to keep going even if it feels slow
So I’m doing it
Still can’t lift my coffee cup one handed though
Mike Smith
It is imperative to underscore the clinical significance of targeted resistance training as the sole evidence-based modality for the rehabilitation of corticosteroid-induced myopathy. The physiological mechanisms of muscle fiber atrophy necessitate a structured, progressive, and supervised intervention protocol to mitigate functional decline. Failure to implement such protocols may result in irreversible loss of independence.
Kitty Price
My mom’s on prednisone and she’s been struggling to get up from her recliner. I’m sending her this. 💪❤️
Aditya Kumar
Why bother reading all this? Just take the pills and sit down.
Colleen Bigelow
They’re poisoning us with steroids and calling it medicine. Next they’ll say our bones are fake and our blood is government syrup. Wake up people. This isn’t science-it’s control.
Billy Poling
While I appreciate the clinical overview presented herein, I must express concern regarding the omission of potential confounding variables such as concomitant use of statins, beta-blockers, and proton pump inhibitors, all of which may independently contribute to proximal myopathy. Furthermore, the absence of a discussion regarding the impact of socioeconomic status on access to physical therapy represents a significant gap in the proposed therapeutic framework. One cannot assume uniform accessibility to rehabilitation services across diverse demographic strata, particularly in rural or underinsured populations. A more comprehensive model would integrate policy-level interventions alongside clinical protocols.
Josias Ariel Mahlangu
My brother had this. Took him two years to figure it out. He’s back to hiking now. PT saved him. Don’t ignore it.
Randolph Rickman
You’re not broken. You’re just adapting to a chemical environment that doesn’t support your body’s natural design. But guess what? Your muscles remember how to be strong. Start small. One rep. One step. One day. You’ve got this.
sue spark
I started PT last month and I can finally reach the top shelf again
It’s not magic
But it’s something