Most people assume generics are just as good as brand-name drugs-and for the vast majority of medications, they are. But there are times when your doctor will write a prescription that says "do not substitute" or "brand medically necessary". If you’ve ever seen that on your prescription, you might wonder: Why? Is this just about profit? Or is there a real medical reason?
When Generics Aren’t Enough
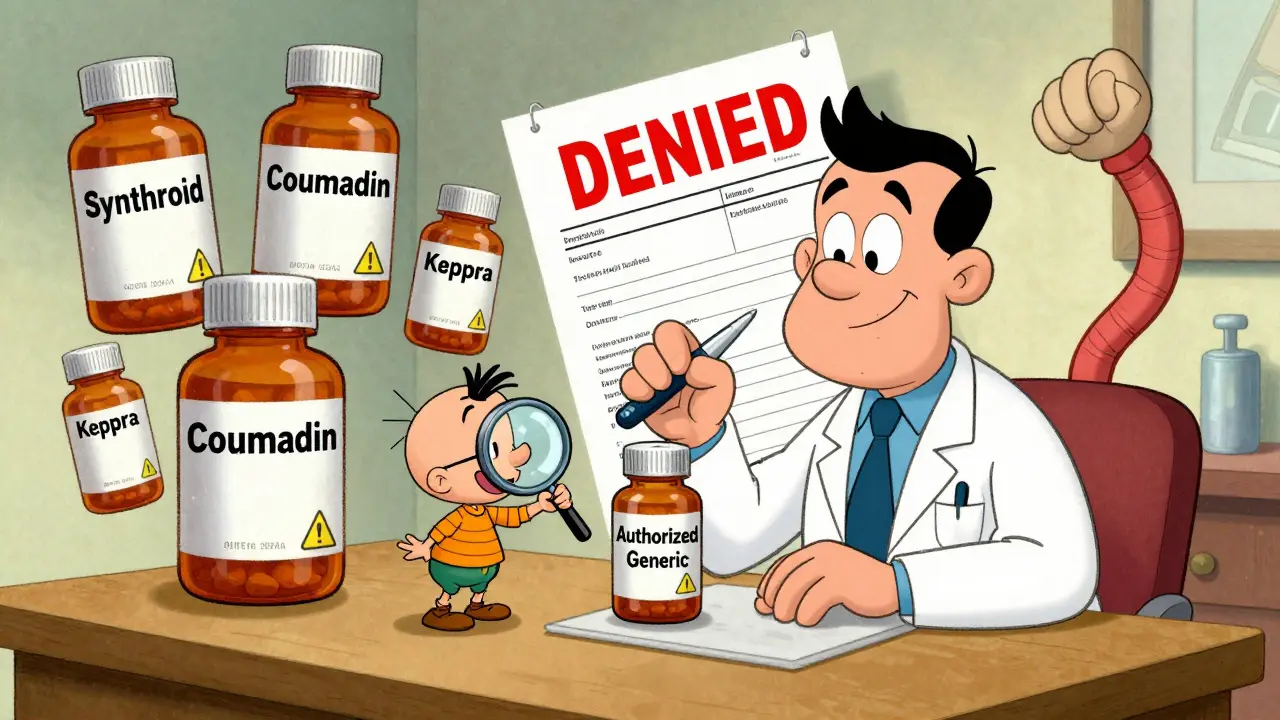
Generic drugs are required by the FDA to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also be bioequivalent, meaning they deliver the same amount of drug into your bloodstream within an 80% to 125% range of the brand. Sounds perfect, right? But for some drugs, even that small window can be dangerous. Drugs with a narrow therapeutic index (NTI) are the main exception. These are medications where a tiny change in blood levels can mean the difference between treatment working and something serious happening-like a seizure, a blood clot, or thyroid failure. Examples include:- Levetiracetam (Keppra) for epilepsy
- Warfarin (Coumadin) for blood thinning
- Levothyroxine (Synthroid) for thyroid replacement
What the Data Shows
A 2019 study in Epilepsy & Behavior followed 1,200 people with epilepsy who were switched from brand-name levetiracetam to a generic version. Nearly 13% had breakthrough seizures after the switch. Only 4.3% of those who stayed on the brand had seizures. That’s a threefold increase. For most other drugs-like statins, blood pressure meds, or antibiotics-there’s no meaningful difference. A 2020 JAMA meta-analysis of over 112,000 patients found brand and generic versions performed identically for drugs like lisinopril, metformin, and atorvastatin. So why do some doctors still prescribe brand-name only for these? Sometimes, it’s habit. A 2018 study from Stanford found doctors who say “Keppra” instead of “levetiracetam” are more likely to prescribe the brand, even when there’s no clinical reason. Drug reps reinforce this by training doctors to think of the brand as the “real” drug.When Inactive Ingredients Matter
Generics have the same active ingredient, but they can use different fillers, dyes, or binders. For most people, this doesn’t matter. But for some, it does. A patient with celiac disease might react to a generic version of ciprofloxacin that uses wheat-based starch. Someone with a shellfish allergy might get sick from a capsule made with gelatin from shellfish. A person with severe lactose intolerance might have stomach cramps from a generic pill that uses lactose as a filler. These cases are rare-but they’re real. The Institute for Safe Medication Practices lists them as one of the three legitimate reasons to prescribe brand-name only. If you’ve had a bad reaction to a generic before, tell your doctor. Document it. That’s your proof.
Insurance and Cost: The Hidden Pressure
Brand-name drugs cost, on average, 80-85% more than generics. In 2022, the average retail price for a brand-name prescription was $471.67. The generic? $13.76. If your doctor writes “brand medically necessary,” your insurance might still refuse to pay unless they approve it first. That’s called prior authorization. It can take up to 72 hours. And even then, approval rates vary. For antiepileptics, insurers approve 89% of requests. For proton pump inhibitors like omeprazole? Only 45%. Patients who get stuck with brand-name prescriptions without approval often pay hundreds more out of pocket. A 2021 Kaiser Family Foundation survey found 42% of patients paid significantly more when their doctor prescribed a brand unnecessarily. And here’s the irony: generics make up 90% of all prescriptions filled in the U.S., but only 23% of total drug spending. That means the system is built to save money-when doctors let it.What You Can Do
If your doctor prescribes a brand-name drug, ask:- Is this a narrow therapeutic index drug?
- Have I had a bad reaction to a generic before?
- Is there a documented reason, or is this just how it’s always been done?
The Bigger Picture
The U.S. spends billions more on brand-name drugs than necessary. Experts like Dr. David Ouyang from Stanford and Dr. Caleb Alexander from Johns Hopkins say up to 97% of brand-only prescriptions could be avoided. That’s not just waste-it’s money that could go toward care for people who actually need it. But change is slow. Drug companies spend billions marketing brand names. Doctors are busy. Insurance rules are confusing. Patients are scared to ask. The good news? More states are requiring electronic prescribing systems to flag when a generic is available. The FDA now requires generic pills to look more like the brand-to reduce confusion. And authorized generics-made by the original brand company but sold under a generic label-are becoming more common. These avoid the variability between different generic manufacturers.Bottom Line
Most of the time, generics are safe, effective, and cheaper. But for a small group of drugs-and a small group of patients-brand-name only is the right choice. It’s not about brand loyalty. It’s about precision. If your doctor prescribes a brand-name drug, ask why. If they say “because it’s better,” push back. Ask for the evidence. If they say “because I’ve seen patients do worse on generics,” ask which ones. If they can’t answer, it might be time to get a second opinion. Your health isn’t a marketing campaign. It’s a science. And you have the right to understand the science behind your prescription.Can a pharmacist switch my brand-name prescription to a generic without my doctor’s permission?
In 49 U.S. states and Washington D.C., pharmacists can substitute a generic unless the doctor writes "do not substitute," "dispense as written," or "brand medically necessary." Texas has different rules for certain drugs. Always check your prescription label-your pharmacist should also notify you if they made a switch.
Why do some people feel worse on generic thyroid medication?
Levothyroxine has a narrow therapeutic index. Even small differences in absorption between generic versions can affect thyroid hormone levels. Some patients report fatigue, weight gain, or depression after switching. The American Thyroid Association recommends staying on the same brand-preferably Synthroid or Tirosint-to avoid these fluctuations. If you feel worse after switching, tell your doctor and ask to go back.
Are generic seizure medications less effective?
For some patients, yes. A 2019 study found 12.7% of people switched from brand-name levetiracetam to generic had breakthrough seizures, compared to 4.3% who stayed on the brand. The FDA allows generics to vary by up to 20% in absorption-but for epilepsy, that’s too risky. Many neurologists recommend sticking with one brand unless there’s a strong reason to switch.
Can I ask my doctor to prescribe a generic even if they usually prescribe the brand?
Absolutely. You have the right to ask. Say something like, "I’ve heard generics are just as good for most drugs. Is there a reason you’re prescribing the brand?" If your condition isn’t one with a narrow therapeutic index, and you’ve never had a bad reaction, there’s likely no medical reason not to switch. Many people save hundreds or thousands per year.
What’s an authorized generic, and is it better?
An authorized generic is made by the original brand company but sold without the brand name. It’s identical to the brand in every way-same active ingredient, same inactive ingredients, same factory. It’s often cheaper than the brand and avoids the variability you might get from third-party generics. Ask your pharmacist if one is available for your medication.

Gregory Parschauer
Let me get this straight - we’re still having this conversation in 2025? The FDA’s bioequivalence standards are a joke when it comes to NTI drugs. I’ve seen patients on levothyroxine go from euthyroid to myxedema coma because some pharmacy tech decided ‘Synthroid is overpriced.’ This isn’t about cost savings - it’s about institutional negligence disguised as efficiency. If your life depends on a 0.025mg precision, don’t let a pharmacist gamble with your thyroid.
And don’t even get me started on the pharma reps whispering ‘Keppra is the gold standard’ into doctors’ ears while they’re too tired to check the Orange Book. It’s not habit - it’s corruption wrapped in white coats.
Anny Kaettano
I’m a nurse practitioner and I’ve had patients come in crying because their generic levetiracetam made them feel like they were drowning in slow motion. One woman had three seizures in two weeks after switching - she was terrified to drive, to hold her baby, to sleep. We went back to Keppra and her life returned.
Generics work for 95% of meds. But for NTI drugs? It’s not ‘maybe’ - it’s ‘don’t risk it.’ I now automatically flag levothyroxine, warfarin, and antiepileptics in my EHR with a red sticky note. No exceptions. Your body doesn’t care about formulary tiers - it only cares about consistency.
Kimberly Mitchell
So let me understand - you’re telling me that a pill made in India with different fillers could cause seizures? That’s insane. And yet we let insurance companies dictate this? This isn’t medicine - it’s a casino run by accountants. I’m not paying $470 for a pill just because some doctor is too lazy to write ‘do not substitute.’ But I’m also not risking my life for $13.76. The system is broken and everyone’s too scared to fix it.
Angel Molano
Stop pretending generics are dangerous. 97% of patients do fine. You’re fearmongering. If you can’t tolerate a generic, get tested for malabsorption - not because the pill changed, but because you’re neurotic.
Clay .Haeber
Oh wow. A 20% absorption variance is ‘too risky’ for seizures but perfectly fine for your 200mg of lisinopril? What’s next - are we going to require custom-made aspirin for each person’s unique aura? This is the kind of pseudoscientific hysteria that makes me want to move to a country where people still believe in germs and not in ‘thyroid trauma.’
Also, ‘authorized generics’? Sounds like the pharmaceutical industry’s way of charging $400 for the same pill with a different sticker. Congrats, you just invented a new tax on gullibility.
Avneet Singh
As someone who’s worked in pharmacoeconomics in Mumbai, I find this entire debate quaint. In India, generics are the norm - even for warfarin. We don’t have the luxury of brand loyalty. The truth? Most patients don’t notice a difference. The ones who do? Often have anxiety disorders masquerading as pharmacological sensitivity. The real issue is not bioequivalence - it’s the placebo effect amplified by American medical theater.
Adam Vella
The epistemological framework underpinning the generic substitution debate is predicated upon a false dichotomy between cost-efficiency and clinical efficacy. The FDA’s bioequivalence parameters, while statistically valid for population-level outcomes, fail to account for individual pharmacokinetic variance - particularly in the context of narrow therapeutic index agents. The empirical data from the 2019 Epilepsy & Behavior study, while compelling, does not establish causation - only correlation - and is confounded by adherence variability and pharmacogenomic heterogeneity.
Furthermore, the conflation of patient-reported outcomes with objective biomarkers introduces a significant bias. The subjective experience of fatigue or depression may be attributable to psychosocial factors, including the nocebo effect, rather than pharmacodynamic instability. Therefore, the blanket recommendation to retain brand-name prescribing for NTI drugs constitutes an overreach that undermines the principles of evidence-based pharmacotherapy and fiscal responsibility.
Angel Tiestos lopez
bro. i had a friend switch from synthroid to generic and she went from ‘i can run marathons’ to ‘i sleep 14 hours and cry at commercials’ 😭
it’s not in her head. it’s in her thyroid. and no, i don’t care if it’s ‘only’ 20% different - if your body’s a precision instrument, you don’t swap out the tuning fork for a cheap knockoff.
also, authorized generics are the real MVP. same pill, less $$$, no drama. ask your pharmacist. they’re the unsung heroes of this whole mess 🙌
Robin Williams
Here’s the truth nobody wants to say: doctors don’t prescribe brand-name because they’re greedy or lazy - they do it because they’ve seen people break. I’ve had patients die from undiagnosed hypothyroidism after a generic switch. Their charts said ‘normal TSH’ - but their bodies screamed otherwise. We’re not talking about headaches. We’re talking about neurological collapse, heart failure, suicide risk.
Generics saved millions. But some medicines aren’t commodities. They’re lifelines. And if your insurance won’t cover the lifeline? That’s not your fault. That’s the system’s failure. Fight for your health - not because you’re special, but because you deserve to be whole.