Half of all people with gallstones never feel a thing. But if you’ve had that sudden, sharp pain under your right ribs-so bad you couldn’t sit still, couldn’t breathe, couldn’t wait for it to pass-you know how quickly silent gallstones can turn into a medical emergency. This isn’t just indigestion. It’s your gallbladder screaming because a stone is blocking the flow of bile. And if it keeps happening, surgery isn’t just an option-it’s the most reliable way to stop the cycle.
What Happens When a Gallstone Gets Stuck
Biliary colic is the name for the pain you feel when a gallstone temporarily blocks the cystic duct. It doesn’t come on slowly. One minute you’re fine; the next, you’re doubled over. The pain starts in the upper right abdomen or just below your breastbone, often spreading to your right shoulder or back. It’s steady, not crampy, and doesn’t get better with burping, pooping, or vomiting. It hits hard within an hour and usually lasts between one and five hours, then fades as the stone shifts.
Most gallstones are made of cholesterol-about 80% in Western countries. The rest are pigment stones, formed from excess bilirubin. They form when bile becomes too concentrated, either because your gallbladder doesn’t empty well or your liver dumps out too much cholesterol. And while 10-15% of adults have them, 80% live with them without knowing. The real danger isn’t the stone itself-it’s what happens when it stays stuck.
When Biliary Colic Turns Into Cholecystitis
If a stone blocks the duct for more than a few hours, the gallbladder starts to swell and get inflamed. That’s acute cholecystitis. It’s not just pain anymore. You’ll likely have a fever, nausea, vomiting, and tenderness so severe that even a light touch hurts. Your skin might turn yellow if the stone moves into the common bile duct and blocks bile from reaching your intestines. That’s jaundice. Or worse-it can trigger pancreatitis if the stone blocks the pancreatic duct.
One in five people who have biliary colic will develop cholecystitis. And without treatment, 20-30% of people with symptomatic gallstones end up in the ER within five years. That’s not a small risk. It’s a ticking clock.
Why Painkillers Aren’t the Answer
Doctors often give NSAIDs like ketorolac or narcotics like meperidine to ease the pain during an attack. Studies show both work equally well at reducing pain-but NSAIDs have fewer side effects. That’s important. Pain relief doesn’t fix the problem. It just buys time. And time is the enemy here.
More than 90% of people who have one episode of biliary colic will have another within 10 years. Two out of three will have another within just two years. Each episode increases the chance of complications. You can’t outwait this. Medication won’t dissolve the stones permanently. And waiting only makes surgery harder.
The Gold Standard: Laparoscopic Cholecystectomy
For anyone with repeated symptoms, removing the gallbladder is the only cure. And the best way to do it? Laparoscopic cholecystectomy. This is keyhole surgery. Surgeons make four tiny cuts in your abdomen, insert a camera and tools, and remove the gallbladder through one of them. It’s not new-it’s been the standard for decades. But it’s still the most effective option.
Here’s what you can expect: hospital stay of about 1.2 days on average, compared to nearly five days for open surgery. Recovery takes about a week, not a month. Most people go back to work in seven to ten days. The complication rate? Below 2% in experienced hands. Patient satisfaction? Around 95%.
Some people wonder if they can avoid surgery. There are alternatives. Ursodeoxycholic acid can dissolve small cholesterol stones-but only in 30-50% of cases, and it takes six months to two years. Even then, half the stones come back within five years. Shock-wave therapy breaks up stones, but it’s rarely used now because recurrence is so high. These aren’t cures. They’re temporary fixes for people who truly can’t have surgery.
Who Should Skip Surgery?
Surgery isn’t risk-free. For healthy people under 75, the benefits far outweigh the risks. But for older adults-especially those over 75 with heart disease, diabetes, or lung problems-the numbers flip. Thirty-day mortality jumps from 0.1% in healthy patients to nearly 3% in those with three or more serious health conditions. That’s not a small difference. It’s life or death.
That’s why doctors now assess risk carefully. If you’re 80, have multiple chronic illnesses, and your symptoms are mild, watchful waiting might make sense. But if you’re 50, active, and your pain is wrecking your life? Surgery isn’t just safe-it’s the best gift you can give your future self.
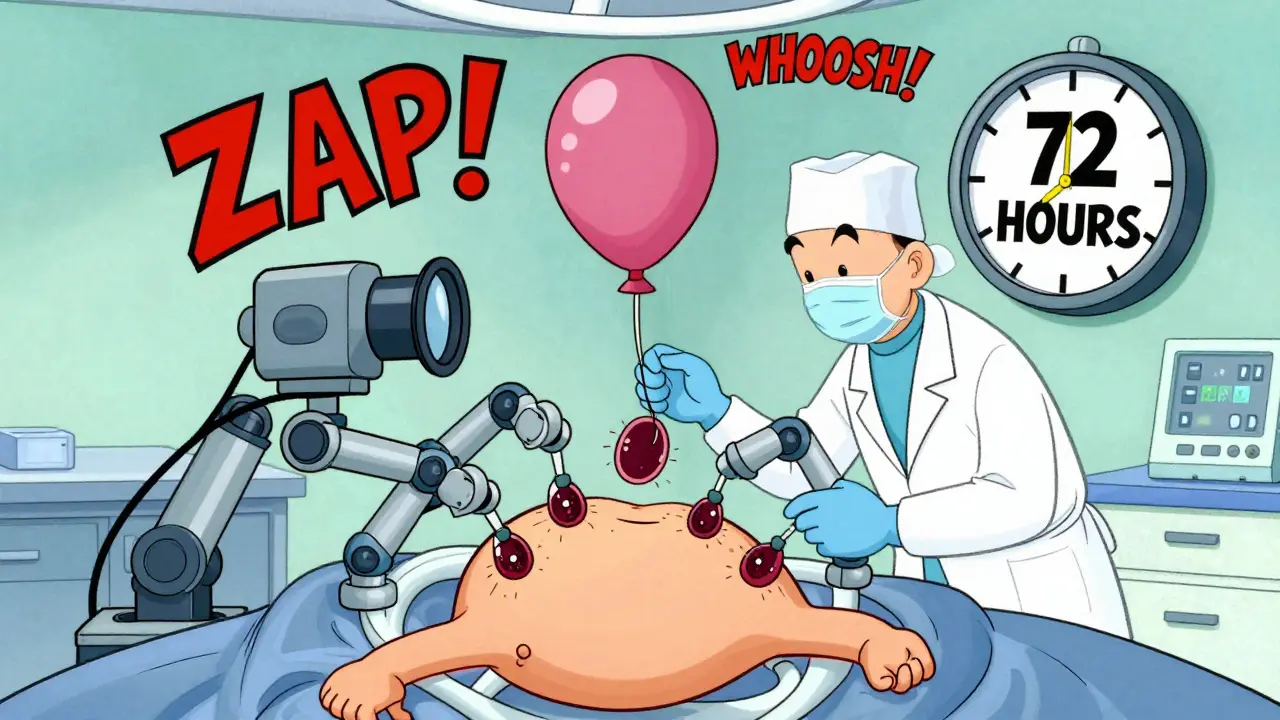
Timing Matters: The 72-Hour Rule
If you’re diagnosed with acute cholecystitis, don’t wait. The Society of American Gastrointestinal and Endoscopic Surgeons recommends surgery within 72 hours. Why? Because the longer you wait, the more inflamed the gallbladder gets. That makes laparoscopic surgery harder. The chance of needing to switch to open surgery? Drops from 25% to just 7% when you operate early.
Early surgery also means fewer days in the hospital, fewer antibiotics, and less risk of the infection spreading. Waiting for the inflammation to “cool down” used to be standard. Now, it’s outdated. If you’re admitted with cholecystitis, push for a surgical consult right away.
What to Expect After Surgery
Most people feel better almost immediately. The pain is gone. No more midnight emergencies. No more avoiding fatty foods for fear of an attack.
But not everyone feels perfect. About 12% have ongoing diarrhea, especially after big meals. That’s because without a gallbladder, bile flows continuously into the intestine instead of being stored and released in bursts. Most people adjust within weeks. A small number-around 6%-get what’s called post-cholecystectomy syndrome: persistent pain, bloating, or nausea. That’s rare, and usually linked to another issue like a bile duct stone or Sphincter of Oddi dysfunction.
One woman, 45, had 17 attacks over 18 months before surgery. Within 10 days after her operation, the pain vanished. Two weeks later, she was back to hiking. That’s the story you want.

The Bigger Picture: Who Gets Gallstones?
Women are two to three times more likely to get them than men. Why? Estrogen boosts cholesterol in bile. Pregnancy, birth control, and hormone therapy all raise the risk. Obesity is another major driver. Nearly 40% of U.S. adults are obese-up from 30% in 2010. That’s why gallstone rates are climbing. Hispanic populations have a 45% higher incidence than non-Hispanic whites, likely due to genetic and dietary factors.
And it’s expensive. About 700,000 gallbladder removals happen in the U.S. every year. That’s $6.2 billion in costs. The global market is growing fast-projected to hit $2.7 billion by 2028. But money isn’t the point. The point is quality of life.
What’s New in Gallstone Care?
There’s a new option for high-risk patients who can’t have surgery: endoscopic ultrasound-guided gallbladder drainage. It’s not a cure, but it can relieve infection and buy time. It’s already helping patients who were told they were too sick for surgery.
Also gaining traction: enhanced recovery after surgery (ERAS) protocols. These are standardized steps-getting patients up and walking within four hours, starting liquids within six, minimizing opioids-that cut hospital stays by 30% and reduce readmissions by 25%. Hospitals using them are seeing better outcomes across the board.
Single-incision laparoscopic surgery (SILS) sounds appealing-just one small cut instead of four. But it’s trickier. Complication rates are 20% higher. Most surgeons stick with the proven multiport method.
One thing’s clear: despite new tools, removing the gallbladder remains the gold standard. As one leading researcher put it, it’s the only treatment that guarantees you’ll never have another attack.
What Should You Do?
If you’ve had one episode of biliary colic:
- Get an ultrasound to confirm gallstones.
- Don’t assume it was a fluke. Recurrence is almost certain.
- Ask your doctor about laparoscopic cholecystectomy.
- If you’re over 75 or have serious health problems, talk about risks vs. benefits.
- If you’re diagnosed with cholecystitis, insist on surgery within 72 hours.
Waiting for the next attack is not a plan. It’s a gamble-and the odds are stacked against you.

Terri Gladden
I had one of those attacks last year and thought I was dying. Like, actually thought I was having a heart attack. Turned out it was a stone the size of a grape. Surgery was scary but worth it. Now I eat tacos every damn day and don't look back.
en Max
The clinical data presented here is both robust and clinically actionable. Biliary colic, as a symptom complex, is frequently misdiagnosed as gastroesophageal reflux or cardiac ischemia; however, the absence of positional or alimentary alleviation is a key discriminant. Laparoscopic cholecystectomy remains the definitive intervention for recurrent episodes, with a morbidity profile that is statistically superior to non-operative management over a five-year horizon.
Jacob Milano
Man, I used to think gallstones were just old people problems. Then my cousin, 32, got hit with one during a family BBQ. She was screaming, clutching her side like someone stabbed her. Turned out she had like six stones. Now she’s back to rock climbing and eating buttered toast like a boss. Surgery isn’t scary-it’s freedom.
Allen Ye
There’s a deeper truth here that our medical-industrial complex refuses to acknowledge: the gallbladder isn’t a useless organ-it’s a precision instrument. We remove it like it’s a broken toaster, but we never ask what happens when the body’s natural rhythm is disrupted. The bile flows constantly now, not in waves. We’ve turned a symphony into a dripping faucet. And yes, most people adapt-but adaptation isn’t healing. It’s survival. We’ve normalized the unnatural because convenience trumps wholeness.
mark etang
This is a critical public health message. Early intervention saves lives, reduces costs, and restores quality of life. All patients presenting with biliary colic must be evaluated for surgical consultation without delay. Procrastination is not a strategy-it is a liability.
Brendan F. Cochran
They say surgery is the answer but what about the big pharma lies? They don’t want you to know about the herbal gallstone flushes. My uncle drank apple cider vinegar and olive oil for a month and pooped out 47 stones. They just don’t want you to know because they make billions off the knife. You’re being played.
jigisha Patel
The data regarding recurrence rates is statistically significant, yet the article lacks a discussion on the confounding variables of dietary fat intake post-cholecystectomy. Furthermore, the assertion that 95% patient satisfaction is universally applicable is methodologically unsound without stratification by BMI, age, or comorbidities. This is oversimplification disguised as education.
Jason Stafford
This is all a lie. The government and big pharma put stones in people’s gallbladders so they’d need surgery. They’ve been doing it since the 80s. The real cure is magnetic resonance therapy with a copper bracelet and fasting during the full moon. I know because I saw it on a documentary that got pulled off YouTube.
Justin Lowans
I’ve seen patients go from bedridden to hiking Machu Picchu after cholecystectomy. It’s not just a procedure-it’s a rebirth. The fear of surgery is real, but the fear of another attack? That’s the real monster. This article doesn’t just inform-it liberates.
Michael Rudge
Oh wow, another ‘just get your gallbladder out’ article. How original. Did you get this from a pharmaceutical ad? People who’ve never even had a gallstone are now convinced they need surgery because some guy on the internet told them to. You’re not helping-you’re creating anxiety for profit.
Ethan Purser
I’ve been living with silent gallstones for 12 years. I used to think they were just… there. Like a silent roommate. But after reading this, I realized I’ve been grieving my body every time I avoided cheese. I didn’t know I was holding my breath until the pain was gone. Surgery isn’t just medical-it’s emotional. I’m scheduled next week. I’m terrified. But I’m also… free.