Starting a new medication can feel overwhelming. You’re handed a prescription, a bottle with tiny print, and maybe a few instructions-but no one walks you through what to actually do. And if you get it wrong, the consequences can be serious. Every year in the U.S., over 1.3 million people end up in the emergency room because of medication mistakes. Many of those mistakes happen to first-time patients who just don’t know what to ask or where to start.
Why Medication Safety Matters More Than You Think
Medication safety isn’t just about taking your pills on time. It’s about making sure the right drug gets to the right person, in the right amount, at the right time, for the right reason. Sounds simple? It’s not. The CDC reports that 350,000 hospitalizations each year are caused by bad reactions to medications. And here’s the scary part: up to half of those errors are preventable. A 2021 Johns Hopkins study found that medication errors contribute to about 7,000 deaths in U.S. hospitals annually. That’s more than car accidents. The good news? Following basic safety steps can cut your risk of harm by up to 50%. You don’t need to be a doctor to protect yourself-you just need to know what to look for.The Six Rights of Medication Safety
Healthcare providers use a checklist called the “Six Rights” to avoid mistakes. As a patient, you should use it too. Here’s what each one means-and how to make sure it’s followed:- Right patient: Always confirm your name and date of birth when picking up a prescription. Pharmacists should verify this. Don’t assume they know you by sight.
- Right medication: Check the bottle label against your prescription. Does the name match? Does the color and shape of the pill look right? If it looks different from last time, ask why.
- Right indication: Ask: “Why am I taking this?” Some medications have multiple uses. You need to know if this one is for your blood pressure, pain, or something else.
- Right dose: Never use kitchen spoons to measure liquid medicine. A tablespoon varies by 25-50% in volume. Use the dosing cup, syringe, or dropper that came with the bottle.
- Right route: Is it supposed to be swallowed, placed under the tongue, applied to the skin, or injected? Taking a topical cream by mouth can be dangerous.
- Right time: Some meds need to be taken with food. Others must be taken on an empty stomach. Some work better in the morning. Others at night. Ask for specifics.
Keep a Complete Medication List
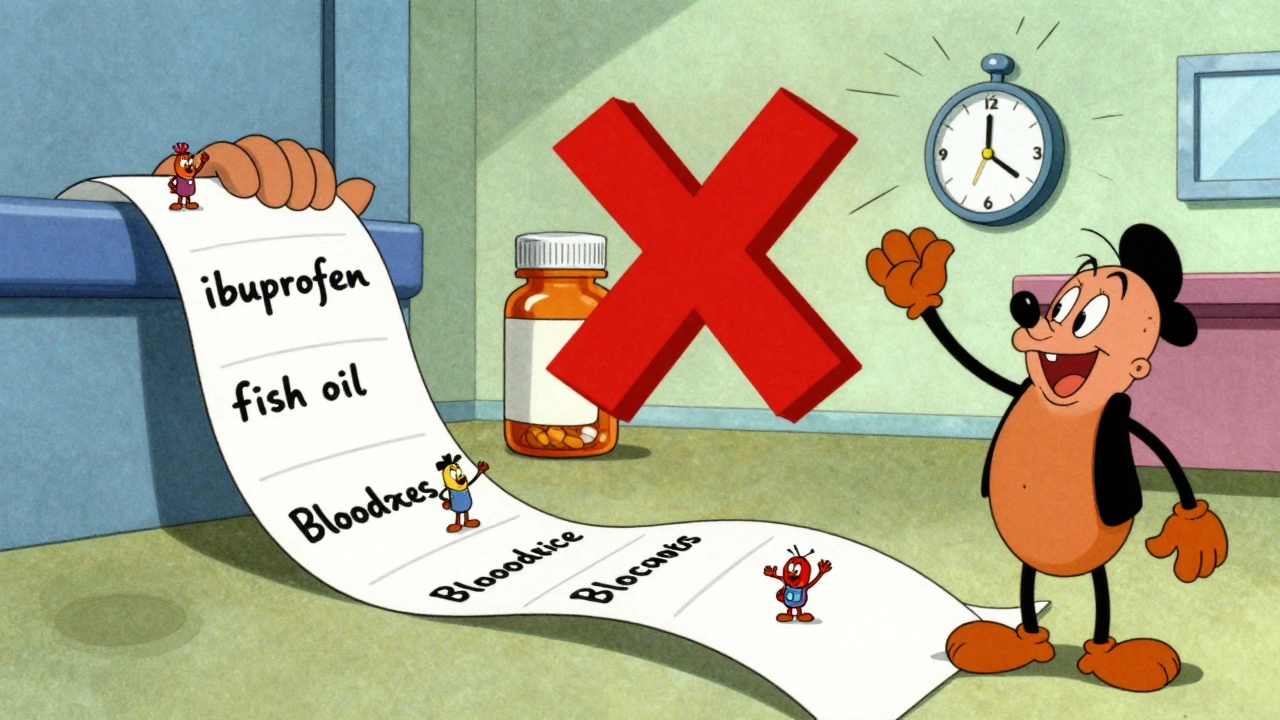
Most people don’t realize how many things they’re taking. Prescription drugs? Yes. But what about ibuprofen? Vitamin D? Fish oil? Herbal teas? All of it counts. The CDC recommends keeping an up-to-date list of everything you take-including the dose and why you take it. Patients who do this have 27% fewer medication errors, according to a 2022 study in the Journal of the American Pharmacists Association. Here’s what to include:- Brand and generic names
- Dosage (e.g., 10 mg, 5 mL)
- Frequency (e.g., once daily, every 6 hours)
- Reason (e.g., “for high blood pressure,” “for joint pain”)
- Prescribing doctor’s name
- Pharmacy name and number
Never Take Someone Else’s Pills
It’s tempting. Your friend says their headache medicine worked great. Your mom says her sleep pill helped her relax. Don’t do it. The FDA says sharing medications causes about 8% of emergency visits for adverse drug events. What works for one person might be dangerous for you. A pill that helps someone’s anxiety might raise your blood pressure. A painkiller that’s safe for them could interact badly with your heart medication. Also, never take expired drugs. Merck’s 2023 safety report found that 18% of medication errors come from using expired pills-especially antibiotics and liquid suspensions. They lose potency and can become toxic.
Read the Label Like Your Life Depends on It
It does. Many errors happen because people read labels in dim light or rush through them. The FDA says 15% of mistakes are caused by misreading labels. Here’s how to avoid that:- Turn on the lights. Use a lamp if needed.
- Hold the bottle up to the light. Check the name, dose, and instructions.
- Look for warnings: “May cause drowsiness,” “Avoid alcohol,” “Take on empty stomach.”
- If you can’t read the print, ask your pharmacist for a large-print label. They’re required to provide it.
Use Tools to Stay on Track
Forgetting a dose is common. Missing a dose of blood pressure or diabetes medicine can be risky. But you don’t have to rely on memory. Medication reminder apps like Medisafe and MyMeds have been shown to improve adherence by 28% among first-time users, according to a 2022 study in the Journal of Medical Internet Research. The best ones let you scan the barcode on your bottle to auto-fill the info. They send alerts, track refills, and even warn you about potential interactions. If you don’t like apps, use a pill organizer. Buy one with compartments for morning, afternoon, evening, and night. Fill it once a week. Set alarms on your phone. Put sticky notes on your mirror. Do whatever works for you.Ask These Three Questions Every Time You Get a New Prescription
You’re not being annoying. You’re being smart. A 2022 study in Patient Education and Counseling found that patients who asked at least three questions about a new medication had 34% fewer side effects in the first month. Here are the three you must ask:- What should I do if I miss a dose? Only 22% of patients ask this. But the answer matters. Some meds you take as soon as you remember. Others you skip. Taking a double dose by accident can be dangerous.
- How should I store this? Forty percent of medications have special storage needs. Insulin must be refrigerated until opened. Some antibiotics must be kept cool. Others should stay dry and away from sunlight. Check the label.
- What side effects should I watch for? Only 65% of pharmacy consultations cover this, according to AHRQ. Know the red flags: chest pain, swelling, trouble breathing, rash, confusion. Don’t wait to see if it “goes away.” Call your doctor right away if something feels wrong.
When in Doubt, Ask Your Pharmacist
Your pharmacist is a medication expert-and they’re often more available than your doctor. CVS Pharmacy, for example, received 3.8 out of 5 stars in 2023 for medication counseling, according to Trustpilot reviews. But many patients don’t take advantage. Walk up to the counter. Say: “I just got this new medicine. Can you explain how to take it?” They’ll show you the label, explain food interactions, and warn you about side effects. No appointment needed. And if they seem rushed? Come back later. Or call. Many pharmacies offer free phone consultations. You deserve clear answers.What If You Make a Mistake?
Everyone slips up. You forget a dose. You take two pills by accident. You realize you’ve been taking your medicine at the wrong time. Don’t panic. Don’t hide it. Call your pharmacist or doctor immediately. Most errors are fixable if caught early. The CDC says reporting mistakes-even small ones-helps improve safety for everyone. Also, if you’re ever given a medication without a label, refuse it. Mislabeling causes 12% of hospital errors, according to ISMP. You have the right to ask: “Is this the right medicine? Is it labeled correctly?”You’re Not Alone
About 66% of Americans take at least one medication. Half take two or more. You’re not weird for feeling confused. A 2023 National Council on Aging survey found that 42% of first-time users struggle with dosing schedules. 37% say labels are too hard to read. But you can get through it. Medication safety isn’t about being perfect. It’s about being aware. It’s about asking questions. It’s about writing things down. It’s about trusting your gut when something doesn’t feel right. The learning curve takes about two to three weeks, according to a 2023 University of Michigan study. After that, it becomes routine. And once it does, you’ll feel more in control-less anxious, less overwhelmed. You’re not just taking a pill. You’re managing your health. And you’re capable of doing it safely.What should I do if I accidentally take too much of my medication?
If you take too much, call Poison Control at 1-800-222-1222 immediately. Do not wait for symptoms. Even if you feel fine, some overdoses don’t show signs right away. Keep the medication bottle handy when you call-it helps them give you accurate advice. If you’re dizzy, having trouble breathing, or losing consciousness, call 911.
Can I crush my pills if I have trouble swallowing them?
Not always. Some pills are designed to release medicine slowly. Crushing them can cause a dangerous overdose. Others have coatings that protect your stomach or prevent them from being broken down too early. Always ask your pharmacist before crushing, chewing, or opening a capsule. If swallowing is hard, ask if there’s a liquid form or a different pill you can take.
How do I know if a new medication interacts with my other drugs?
Pharmacists use computer systems to check for interactions when filling prescriptions. But you should still ask. Bring your full medication list to every appointment. Tell your pharmacist everything you take-even supplements like St. John’s Wort or magnesium. Some herbs can interfere with blood thinners, heart meds, or antidepressants. If you’re unsure, ask: “Could this new pill react badly with anything else I’m taking?”
Is it safe to take my medication with alcohol?
Many medications shouldn’t be mixed with alcohol. It can increase drowsiness, raise blood pressure, damage your liver, or make the drug less effective. Check the label. If it says “avoid alcohol,” don’t drink. Even a single glass can be risky with painkillers, antibiotics, anxiety meds, or sleep aids. When in doubt, ask your pharmacist.
Why do I need to take this medicine even if I feel fine?
Some medications treat conditions you can’t feel-like high blood pressure, high cholesterol, or diabetes. Stopping them because you feel okay can lead to serious problems later: heart attack, stroke, kidney damage. Your doctor prescribed it to prevent future illness, not just to treat current symptoms. Don’t stop unless your doctor tells you to.

Shubham Pandey
Just took my blood pressure pill and realized I didn’t read the label. Oops. Thanks for the reminder.
Elizabeth Farrell
I know this sounds basic, but I’ve seen so many elderly relatives panic over pill changes-color, shape, size-and assume they’ve been given the wrong medicine. It’s not paranoia, it’s fear. And honestly? Pharmacists should proactively say, ‘Hey, this is a generic, it looks different but works the same.’ No one should have to Google their meds at 2 a.m. I keep a printed list in my wallet now. It’s saved me twice. You’re not being annoying-you’re being alive.
Sheryl Lynn
Oh, darling, the ‘Six Rights’? How quaint. In my circle, we refer to it as the ‘Pharmacological Tetris’-you’re juggling bioavailability, CYP450 interactions, and circadian pharmacokinetics while trying not to vomit from the sugar-coated placebo they call ‘ibuprofen.’ And don’t get me started on the FDA’s definition of ‘readable font.’ If you need a magnifying glass and a UV lamp to decipher your prescription, you’re not a patient-you’re a test subject in a Kafkaesque bureaucracy. Also, ‘medication list’? Please. I maintain a color-coded, blockchain-verified, QR-coded dossier. Because if you’re not documenting your pharmaceutical journey like a medieval alchemist, are you even living?
Paul Santos
Medication safety is just the tip of the iceberg, man. We’re living in a post-pharmaceutical society where the body is a system of cascading feedback loops, and every pill is a node in a vast, unregulated network of corporate interests and placebo-driven cognition. 🤔 I once took a melatonin pill that tasted like regret and existential dread. Turns out it was expired. The real drug? The fear we’re all conditioned to swallow without question. #Pharmakon #DerridaWasRight
Eddy Kimani
Just wanted to add-when you're on multiple meds, always check interactions on Medscape or Epocrates. Not just the pharmacy app. I had a patient on warfarin who started taking turmeric supplements. INR spiked to 8.3. No symptoms at first. Then he woke up with a subdural. Pharmacies don't always catch everything, especially with herbs. Always cross-reference. And yes, St. John’s Wort is a sneaky one-it turns SSRIs into a firework.
Chelsea Moore
THIS IS WHY AMERICA IS FALLING APART!! People don’t READ LABELS!! I had a neighbor take her daughter’s ADD meds because she was ‘tired’-and now she’s in rehab!! And the pharmacies? They don’t even check!! I called the FDA, I called the mayor, I called my congressperson-NO ONE CARES!! You think this is about pills? It’s about MORAL DECAY!! We’ve become a nation of lazy, label-ignoring zombies!! I’m crying right now!! 😭😭😭
John Biesecker
Man, I just realized I’ve been taking my antidepressant with grapefruit juice for 3 years 😅 whoops. I thought it was ‘healthy.’ Now I’m scared to even drink water. But honestly, this post made me feel less alone. I used to think I was dumb for needing reminders. Turns out, the system’s just broken. Thanks for writing this. Also, I’m gonna start using Medisafe. And maybe a pillbox. And maybe write ‘DO NOT EAT THIS’ on the bottle. 🤷♂️💊
Genesis Rubi
USA still has the best healthcare system in the world. If you can't read a label, that's your fault. You think Canada or Germany would let you live like this? No. They'd lock you up. We have the best doctors, the best pharmacies, the best science. If you're confused, maybe you're not smart enough to handle meds. Just stop complaining. And stop taking those herbal teas-they're just hippie poison. 💪🇺🇸
Doug Hawk
Biggest thing I learned after my heart surgery? Never trust memory. Always write it down. I kept a notebook with names, times, side effects, and who I talked to. I even noted the pharmacist’s name. One time I caught a misfill because I remembered the last bottle had a different cap color. No one asked me to do that. I just did. If you’re on meds, treat it like a job. You’re the CEO of your own body. No one else is going to run it for you.
John Morrow
Let’s be real-the entire pharmaceutical industry is a Ponzi scheme built on placebo effects and regulatory capture. The ‘Six Rights’? A PR stunt to make you feel safe while they profit off your dependency. The CDC data? Cherry-picked. The Johns Hopkins study? Funded by Big Pharma. You think your ‘medication list’ protects you? It’s just another data point in your digital dossier. You’re not managing your health-you’re feeding the algorithm. And the real danger isn’t the pill you miss-it’s the one you never knew you were prescribed.
Kristen Yates
In my village in rural Kenya, people share medicine all the time. No labels. No pharmacies. Just trust, experience, and elders. We don’t have apps or pill organizers. But we don’t have 1.3 million ER visits either. Maybe the answer isn’t more documentation-it’s more community. I’ve seen people heal with tea, prayer, and a hand on the forehead. Don’t forget that. Technology helps, but connection heals.
Saurabh Tiwari
Bro i just took my meds with coffee and now i feel like a robot 😅 but hey at least i know what i'm taking now. thanks for the post. gonna start using the app. also why do pills always look like candy? i almost ate my blood pressure one last week
Michael Campbell
They’re putting fluoride in the water and now they want you to swallow pills? Coincidence? I don’t think so. The government wants you docile. The pharmacy? They’re just middlemen. The real drug? Control. You think you’re safe because you read the label? You’re just following the script. Wake up. That ‘medication list’? It’s a tracker. They know what you take. They know when you skip. They’re watching.
Victoria Graci
There’s something deeply poetic about the ritual of medication-the way we turn tiny chemical miracles into daily prayers. We swallow our fears in capsules. We measure our hope in milligrams. And yet, we’re told to trust a system that’s as fallible as we are. The ‘Six Rights’ aren’t just a checklist-they’re a contract between vulnerability and care. I keep my list in a leather journal. Each entry feels like a vow. Not because I’m afraid of dying, but because I’m determined to live-on my terms, with my eyes open.
Saravanan Sathyanandha
As a healthcare worker in India, I’ve seen patients take antibiotics meant for their children, skip doses because they ‘feel better,’ and avoid asking questions out of respect for doctors. This guide is not just helpful-it’s revolutionary in contexts where literacy and access are barriers. I distribute printed versions in clinics. One woman told me, ‘Now I don’t feel stupid when I ask.’ That’s the real victory. Knowledge isn’t privilege. It’s dignity.