Medication-Induced Angioedema Symptom Checker
Check Your Symptoms
This tool helps identify if your symptoms might indicate medication-induced angioedema—a potentially life-threatening reaction to blood pressure medications. Do not rely on this tool for diagnosis. If you have any breathing difficulties, seek emergency care immediately.
Are you currently taking these medications?
Select any symptoms you're experiencing
Additional information
Swelling in your lips, tongue, or throat isn’t just uncomfortable-it can stop you from breathing. When this happens because of a medication you’ve been taking for months or even years, it’s not an allergy you can just treat with an antihistamine. This is angioedema from medications, and it’s more common-and more dangerous-than most people realize.
What Exactly Is Medication-Induced Angioedema?
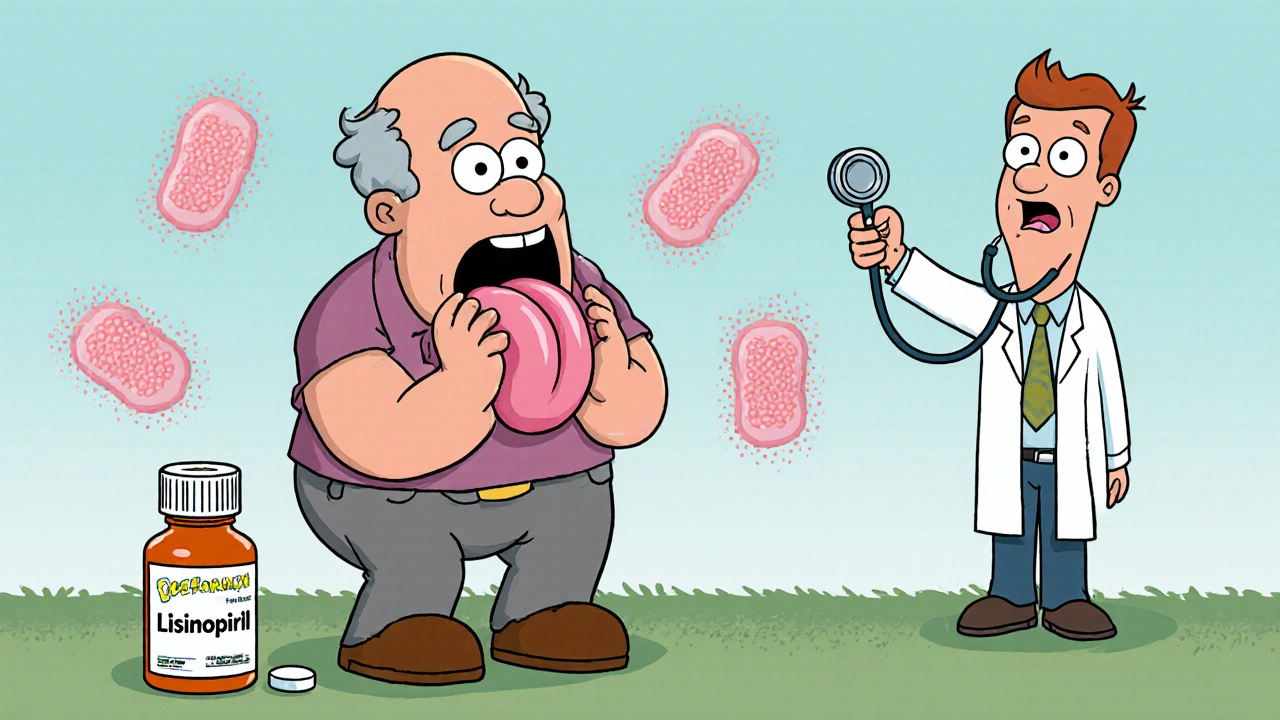
Angioedema is deep swelling beneath the skin or mucous membranes. Unlike hives, which sit on the surface, this swelling happens in the layers below. It can show up on your face, lips, tongue, throat, hands, feet, or even inside your gut. When it hits your airway, it becomes an emergency. You might notice your voice getting hoarse, your tongue feeling thick, or struggling to breathe. In severe cases, you can lose your airway in minutes. The most common trigger? Medications. About 30% to 40% of all drug-induced angioedema cases come from ACE inhibitors-drugs like lisinopril, enalapril, and ramipril, commonly prescribed for high blood pressure and heart failure. These aren’t rare drugs. Around 50 million Americans take them. And while most people tolerate them fine, 0.1% to 0.7% will develop swelling. That sounds small, but with millions of users, it adds up to thousands of cases every year.Two Very Different Types of Swelling
Not all angioedema is the same. There are two main types, and treating them the wrong way can be deadly. Mast cell-mediated (histaminergic) angioedema happens with allergic reactions. Drugs like penicillin, aspirin, or NSAIDs (ibuprofen, naproxen) can trigger it. This type responds to standard allergy treatments: antihistamines like diphenhydramine, steroids like prednisone, and epinephrine if breathing is at risk. It usually comes on fast-within minutes to hours after taking the drug-and often comes with hives or itching. Bradykinin-mediated angioedema is different. It’s caused by ACE inhibitors, ARBs (like losartan), and sometimes other drugs. It doesn’t involve histamine. That means antihistamines and steroids won’t help. Epinephrine? Often useless. This type builds up slowly, over hours, and can strike even after years of safe use. You might not get hives. No itching. Just swelling-sometimes in your throat, sometimes in your belly causing severe pain. The biggest problem? Doctors often mistake bradykinin-mediated angioedema for an allergic reaction. They give you antihistamines and send you home. The swelling doesn’t go down. You come back. And again. One patient in a 2019 Mayo Clinic study waited three years before anyone connected her tongue swelling to her daily lisinopril. By then, she’d lost two teeth from repeated swelling.Who’s at Highest Risk?
Some groups are much more likely to develop medication-induced angioedema. - African-American patients: Up to 2.2% develop swelling on ACE inhibitors-more than three times the average rate. - Women: Twice as likely as men to be affected. - People over 65: Slower metabolism and more medications increase risk. - Those with a history of unexplained facial swelling: Even if it happened years ago, it could be a sign you’re prone to this reaction. And here’s the kicker: You don’t need to be on the drug for long. Most cases happen within the first year, but 1 in 5 happen after two or more years of use. That means if you’ve been on lisinopril for five years and suddenly your lip swells up, it’s not a coincidence. It’s the drug.
When to Go to the ER-Right Now
This isn’t something to wait out. If you have any of these symptoms, call 911 or go to the nearest emergency room:- Swelling of the tongue, throat, or lips that’s getting worse
- Difficulty swallowing or feeling like something’s stuck in your throat
- Hoarse voice, whispering, or inability to speak clearly
- Stridor-a high-pitched wheezing sound when you breathe
- Sudden shortness of breath or feeling like you can’t get air in
- Fainting or dizziness
What Happens After the Swelling?
Once you’re stable, the first step is simple: stop the drug. If it’s an ACE inhibitor, you’re done with it for good. Never take it again. And don’t switch to an ARB (like valsartan or losartan)-there’s a 50% chance you’ll get swelling again. Your doctor should refer you to an allergist or immunologist. They’ll help figure out what caused it. Blood tests aren’t always helpful, but your history and timing matter. If you had swelling after starting a new medication, that’s the likely culprit. For mast cell-mediated cases, you’ll likely be given an epinephrine auto-injector (like an EpiPen) and told to carry antihistamines. For bradykinin-mediated cases, you won’t need those. Instead, you’ll need to know which drugs to avoid forever. That includes ACE inhibitors, ARBs, and sometimes even certain painkillers like NSAIDs.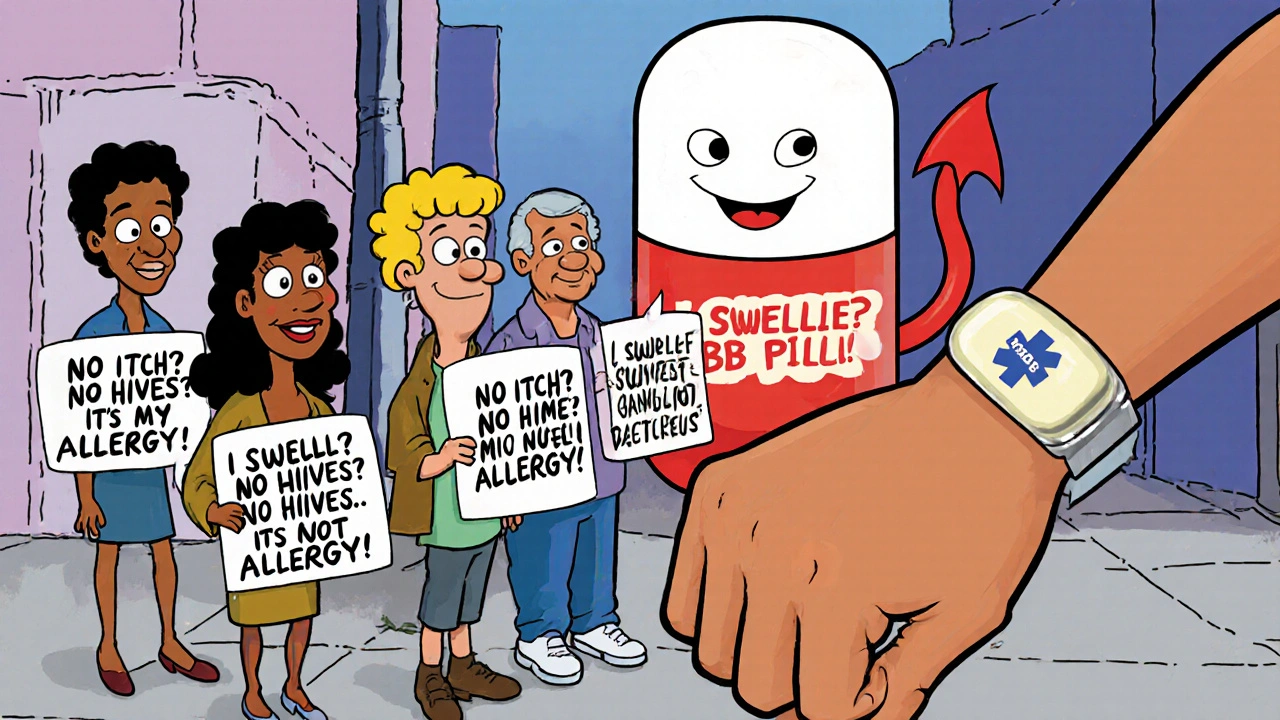
Why Most Treatments Don’t Work
You might hear someone say, “Just take Benadryl and you’ll be fine.” That advice can kill. Bradykinin-mediated angioedema doesn’t respond to antihistamines or steroids because it’s not driven by histamine. It’s caused by too much bradykinin-a chemical that makes blood vessels leak fluid into tissues. The only effective treatments are specific drugs like icatibant (a bradykinin blocker) or C1 inhibitor concentrate. But those are hospital-only, reserved for emergencies. That’s why prevention is everything. If you’ve had one episode, you’re at high risk for another. And if you’re still on an ACE inhibitor after your first episode? You’re playing Russian roulette with your airway. About 15% to 30% of patients have repeat attacks because they weren’t properly warned to stop the drug.What You Can Do Today
If you’re taking an ACE inhibitor or ARB:- Know the signs of swelling-especially if it’s painless and doesn’t itch.
- If you’ve ever had unexplained facial or tongue swelling, tell your doctor. Even if it happened years ago.
- Don’t assume your doctor knows this. Only 45% of primary care physicians correctly identify ACE inhibitors as the #1 drug cause.
- Ask: “Could this swelling be from my blood pressure pill?”
- Carry a list of your medications and a note saying: “Suspected drug-induced angioedema. Avoid ACE inhibitors and ARBs.”
- Wear a medical alert bracelet that says “Drug-Induced Angioedema - Avoid ACEi/ARBs”
- Keep a written action plan from your specialist
- Teach someone close to you how to recognize the signs and when to call 911
The Bigger Picture
Angioedema from medications isn’t rare. It’s underdiagnosed, mistreated, and misunderstood. The global market for angioedema drugs is growing fast-$2.4 billion by 2028-but most of that’s for hereditary forms. For the thousands of people getting swelling from their blood pressure pills, the solution isn’t a new drug. It’s awareness. Doctors need to stop treating all swelling like an allergy. Patients need to know that a silent, painless swelling can be more dangerous than a heart attack. And we all need to stop assuming that if a drug has been prescribed for years, it’s safe. The good news? Once you identify the trigger and stop it, the risk drops to nearly zero. You can live a full, healthy life-just not on that medication.Angioedema isn’t just a side effect. It’s a warning. Listen to your body. Ask the right questions. And if your throat swells-don’t wait. Act.
Scott Macfadyen
Just had this happen to my uncle last year. Took lisinopril for 7 years. One morning his tongue swelled up like a balloon-no hives, no itching, just pure panic. ER docs gave him Benadryl, sent him home. He came back three days later barely able to talk. Turned out to be bradykinin-mediated. They didn’t even test for it until his wife demanded a second opinion. Now he’s on a different med and lives fine. But if you’re on an ACE inhibitor and you’ve ever had unexplained swelling-stop ignoring it. This isn’t ‘maybe allergies.’ This is your throat slowly closing.
Chloe Sevigny
It’s fascinating how medical paradigms persist despite contradictory evidence. The diagnostic inertia surrounding ACE inhibitor-induced angioedema reflects a broader epistemological failure in clinical medicine-where symptomatology is subsumed under the heuristic of ‘allergy’ without sufficient mechanistic inquiry. The absence of histamine-mediated markers is not merely an oversight; it’s a systemic misattribution rooted in pharmaceutical inertia and cognitive bias. We treat the symptom as if it were the cause, and in doing so, we perpetuate iatrogenic harm under the guise of protocol.
Denise Cauchon
Canada’s got it easy. Over here in the States, doctors act like you’re wasting their time if you say your lip swelled up from a pill you’ve taken for years. I had to beg for 3 months before they’d even consider stopping my ramipril. And now? I’m stuck with this stupid medical bracelet. Like I’m some kind of walking hazard. Meanwhile, my neighbor’s husband died because his doc said ‘it’s just allergies’ and gave him more Benadryl. 😤
Andrea Johnston
Wow. So you’re telling me that millions of people are on a drug that can silently choke them to death, and the medical community still treats it like a minor side effect? And you think people are just supposed to ‘ask their doctor’? Please. Most doctors don’t even know what bradykinin is. I’ve seen patients get sent home with a prescription for antihistamines while their tongue swells. This isn’t negligence. It’s negligence dressed up in white coats.
Victoria Malloy
Thank you for writing this. I’ve been scared to tell anyone about my swelling after starting lisinopril last year. Thought I was overreacting. Now I know I wasn’t. I switched meds, got a medical alert bracelet, and even taught my kids what to look for. It’s scary, but now I feel like I’m in control. You’re not alone.
Alex Czartoryski
Oh here we go. Another ‘your blood pressure pill is trying to kill you’ scare piece. Let me guess-next you’ll say coffee causes cancer and sunlight gives you skin cancer. People need to chill. I’ve been on lisinopril for 12 years. No swelling. My mom’s been on it since 1998. She’s 82 and still running marathons. You’re scaring people for clicks. Not everyone’s a walking emergency.
Gizela Cardoso
My sister had this happen after 5 years on enalapril. No warning. No hives. Just woke up one day with her voice gone and couldn’t swallow water. Took 4 ER visits before anyone figured it out. Now she’s on a different med and does fine. But I wish someone had told us earlier. This info saved her life. Please share it with anyone on blood pressure meds.
Premanka Goswami
They don’t want you to know this. Big Pharma doesn’t want you to know that ACE inhibitors cause silent throat death. They’re hiding it behind ‘rare side effects.’ Why? Because they make billions off these pills. And the FDA? They’re in the pocket of the drug companies. They don’t care if you die quietly. They care about quarterly profits. Wake up. This isn’t medicine-it’s corporate murder with a stethoscope.
Alexis Paredes Gallego
Oh, so now it’s ‘bradykinin-mediated’? What’s next? The moon landing was faked and your blood pressure pill is a mind-control tool? I’ve been on lisinopril since 2010-no swelling, no issues. Meanwhile, you people turn every minor puffiness into a biohazard. Maybe your body’s just reacting to gluten, or EM waves, or the government’s chemtrails. Don’t blame the drug. Blame your immune system’s overactive paranoia.
Brandon Lowi
Let me be blunt: if you’re on an ACE inhibitor and you haven’t had your tongue swell up by now-you’re just lucky. Not smart. Not healthy. Lucky. And you know what? That luck runs out. I’ve seen three people die from this. One was my cousin. He got sent home with antihistamines. They told him it was ‘allergic rhinitis.’ He choked on his own tongue while sleeping. No one saw it coming. No one even asked if he was on blood pressure meds. That’s not a tragedy. That’s a crime.
Joshua Casella
I’m the author of this post. Thank you all for your responses. I’ve spent years working in ERs and seen too many people come in with swollen tongues, told it’s ‘just allergies,’ and leave with no answers. I wrote this because I watched a woman lose her teeth because no one connected her swelling to her daily pill. I’m not here to scare you-I’m here to arm you. If you’re on an ACE inhibitor or ARB and you’ve ever had unexplained swelling-even once-stop taking it. Talk to your doctor. Demand a referral. Your life isn’t worth gambling on outdated assumptions. You deserve to breathe. Don’t wait for the next episode to be your last.