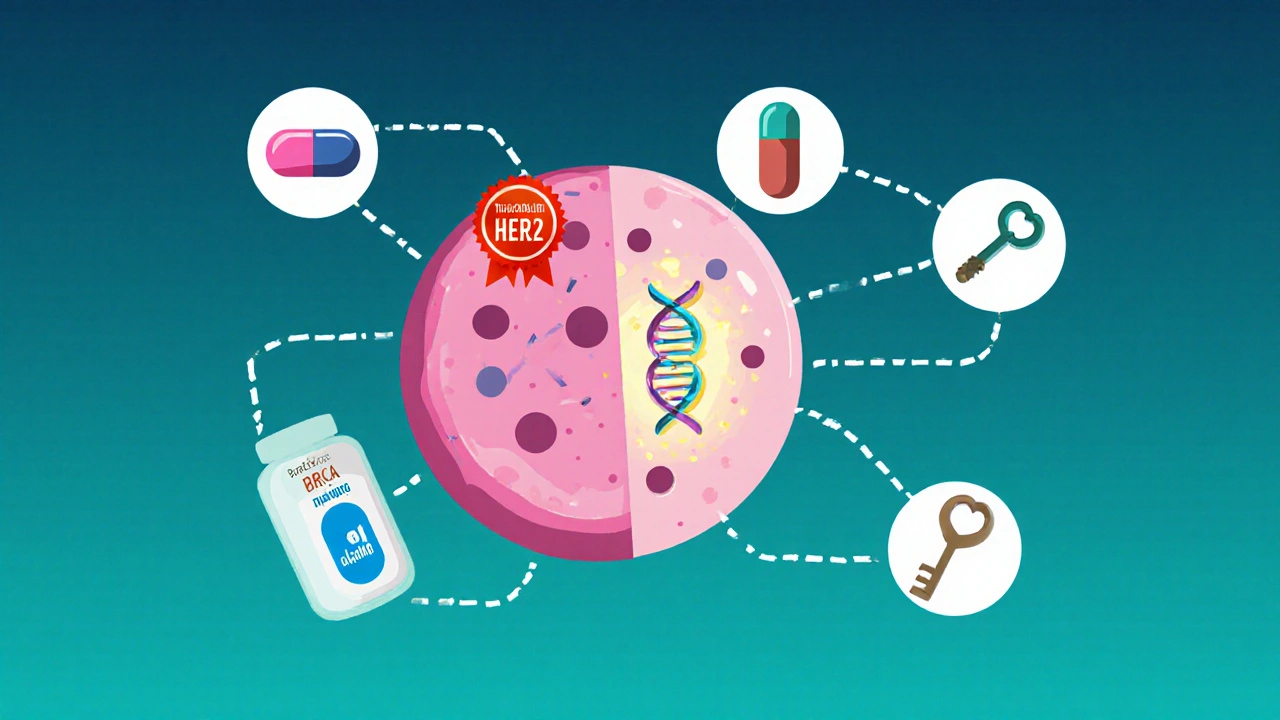
Personalized Breast Cancer Targeted Therapy Selector
HER2 Positive
Overexpression of HER2 protein
Hormone Receptor Positive
Estrogen or Progesterone receptor positive
BRCA Mutation
Mutations in BRCA1 or BRCA2 genes
PI3K Alteration
Mutations in PI3K pathway
CDK4/6 Amplification
Cell cycle checkpoint disruption
No Clear Target
No identifiable molecular driver
Recommended Targeted Therapy Options
Quick Summary
- Targeted therapy attacks cancer’s weak spots instead of blasting all cells.
- Genomic testing decides which drug matches your tumor’s DNA.
- Common targets include HER2, hormone receptors, PI3K, CDK4/6, and PARP.
- Side‑effects are usually milder, but monitoring is still essential.
- Choosing the right regimen follows a simple decision checklist.
What Exactly Is Targeted Therapy?
When it comes to advanced treatment, targeted therapy for breast cancer is a set of drugs designed to block specific molecules that drive tumor growth. Unlike traditional chemotherapy that attacks any rapidly dividing cell, these drugs zero in on a molecular "Achilles' heel"-a protein, gene mutation, or pathway that the cancer relies on.
How Targeted Drugs Do Their Job
Think of a cancer cell as a tiny factory. It needs power, raw materials, and a command center. Targeted agents either cut the power supply, stop the raw material line, or scramble the command signals. For example, a HER2 inhibitor binds to the HER2 protein on the cell surface, preventing the signal that tells the cell to divide. A CDK4/6 inhibitor stalls the cell‑cycle checkpoint, keeping the cell from copying its DNA.
Key Players in Breast‑Cancer Targeting
Below are the most frequently used targets and their corresponding drugs. Each entry includes the first‑time definition with microdata.
- HER2 is a protein that, when over‑expressed, fuels aggressive tumor growth. Drugs like trastuzumab and pertuzumab bind HER2 and flag the cell for immune attack.
- Hormone Receptors (ER/PR) are cell‑surface receptors that respond to estrogen or progesterone, driving many breast cancers. Aromatase inhibitors and selective estrogen‑receptor degraders (SERDs) blunt this hormonal signal.
- PI3K is a kinase that activates growth pathways; mutations make it a common resistance driver. Alpelisib blocks the mutated PI3Kα subunit.
- CDK4/6 controls the "G1‑S" checkpoint in the cell cycle. Inhibitors such as palbociclib, ribociclib, and abemaciclib keep cancer cells from replicating DNA.
- PARP repairs DNA breaks. Tumors with BRCA1/2 mutations rely heavily on PARP, so inhibitors like olaparib cause lethal DNA damage.
- Immunotherapy (PD‑1/PD‑L1) unleashes the immune system by blocking the "off" signal that tumors use to hide.
- Genomic Testing examines tumor DNA for mutations, amplifications, or fusions that indicate a targetable pathway.
- Companion Diagnostic is a lab test approved to predict response to a specific targeted drug.
Traditional Chemotherapy vs. Targeted Therapy: A Quick Comparison
| Aspect | Targeted Therapy | Traditional Chemotherapy |
|---|---|---|
| Mechanism | Blocks specific molecular drivers | Damages DNA of any rapidly dividing cell |
| Side‑Effect Profile | Usually milder; organ‑specific (e.g., heart, liver) | Broad; nausea, hair loss, immune suppression |
| Response Rate | High when the target is present (70‑90% in HER2‑positive) | Variable; often 30‑50% in advanced disease |
| Typical Use | After confirming target via testing; often first‑line for HER2+, HR‑+, BRCA‑mutated | When no targetable mutation is found or in combination with targeted agents |
Who Benefits Most from a Personalized Approach?
Not every breast tumor has a clear target. The decision tree looks like this:
- Get a biopsy and request a comprehensive genomic panel.
- If HER2 is amplified → HER2‑directed antibodies or antibody‑drug conjugates.
- If estrogen/progesterone receptors are positive → hormone‑blocking agents, possibly combined with CDK4/6 inhibitors.
- If a BRCA mutation shows up → PARP inhibitors become an option.
- If PI3K pathway changes appear → PI3K inhibitors are considered.
- If none of the above, chemo or immunotherapy may be the next step.
This logic ensures you’re not getting a drug your tumor can ignore.
Step‑by‑Step Guide to Starting Targeted Therapy
- Ask for a genomic test. Popular panels include FoundationOne CDx and Oncotype DX. Insurance often covers them when the doctor orders a targeted plan.
- Review the report with your oncologist. Look for listed alterations (e.g., HER2+3+, PIK3CAH1047R).
- Match the alteration to an FDA‑approved drug. Use the companion diagnostic list to confirm eligibility.
- Discuss logistics. Some drugs are IV infusions (trastuzumab), others are oral pills (palbociclib). Decide what fits your schedule.
- Start treatment and set up monitoring. Baseline heart echo for HER2 agents, liver tests for PI3K inhibitors, CBC for CDK4/6 blockers.
- Track response. Imaging every 2‑3 months, plus symptom journaling, helps catch progression early.
Managing Common Side Effects
Even though targeted drugs are “gentler,” they still bring their own quirks.
- Heart monitoring. HER2 antibodies can affect cardiac function. A quarterly echocardiogram catches issues before they become serious.
- Diarrhea. PI3K and CDK4/6 inhibitors often upset the gut. Over‑the‑counter loperamide, low‑fiber meals, and staying hydrated are first‑line tricks.
- Blood count drops. Palbociclib can lower neutrophils. Regular CBCs and dose adjustments keep you safe.
- Skin rashes. PARP inhibitors may cause photosensitivity. Sunscreen and protective clothing are a must.
Never ignore a new symptom-call your care team before it escalates.
Checklist: Is Targeted Therapy Right for You?
- Has a comprehensive genomic test been done?
- Is there a documented target (HER2, ER/PR, BRCA, PIK3CA, etc.)?
- Do you meet the companion diagnostic criteria?
- Are you comfortable with the administration route (IV vs. oral)?
- Can you commit to the required monitoring schedule?
If you answered “yes” to most, you’re likely a good candidate for a personalized regimen.
Future Trends: Where Personalized Breast Therapy Is Heading
Research is on a fast track. Some exciting directions include:
- Next‑generation HER2‑targeted antibody‑drug conjugates that deliver chemotherapy directly into the tumor cell, sparing normal tissue.
- Combination immunotherapy plus CDK4/6 blockade - early trials show deeper, longer responses.
- Liquid biopsies that monitor circulating tumor DNA, allowing doctors to switch drugs the moment resistance appears.
- Artificial‑intelligence driven treatment algorithms that weigh dozens of biomarkers to suggest the optimal cocktail.
Staying informed means you can ask your oncologist about clinical trials that fit your molecular profile.
Frequently Asked Questions
How long does a targeted therapy course last?
Most targeted agents are given continuously until the disease progresses or side effects become intolerable. Some, like trastuzumab, may be stopped after a predefined number of cycles if imaging shows a complete response.
Can I combine targeted therapy with chemotherapy?
Yes, many protocols pair a HER2 antibody with taxane‑based chemo for an upfront “dual‑attack.” The schedule is decided by the oncologist based on tumor burden and patient health.
Are targeted drugs covered by insurance?
Most major insurers cover FDA‑approved targeted agents when a documented biomarker is present. Pre‑authorization often requires the genomic report and a note from the treating physician.
What happens if my tumor develops resistance?
Resistance is common after 12‑18 months. Liquid biopsy can spot new mutations; doctors may then switch to a different class (e.g., from a HER2 antibody to a HER2‑drug conjugate) or add another agent like a CDK4/6 inhibitor.
Is targeted therapy safe during pregnancy?
Most targeted agents are contraindicated because they can cross the placenta and affect fetal development. If you are planning a pregnancy, discuss alternative timing or options with your oncologist.

Paul Koumah
If you think DNA testing is optional, you’re basically guessing your way through chemo.
Erica Dello
Honestly, many patients ignore the basic guidelines 🙄 they should get a genomic panel before any treatment 🙃
sara vargas martinez
Targeted therapy has fundamentally changed the therapeutic landscape for breast cancer patients; it allows clinicians to focus on molecular drivers rather than indiscriminately attacking all dividing cells.
The initial step involves comprehensive genomic profiling, which can identify alterations such as HER2 amplification, estrogen receptor positivity, BRCA mutations, PI3K pathway mutations, and CDK4/6 amplifications.
When HER2 is overexpressed, monoclonal antibodies like trastuzumab and pertuzumab are administered, often in combination with chemotherapeutic agents to enhance response rates.
Hormone‑receptor positive tumors benefit from aromatase inhibitors or selective estrogen‑receptor degraders, and the addition of CDK4/6 inhibitors such as palbocicline further extends progression‑free survival.
Patients harboring germline BRCA1 or BRCA2 mutations are candidates for PARP inhibitors, which exploit synthetic lethality to induce DNA damage in cancer cells while sparing normal tissue.
PI3K‑mutated cancers can be treated with alpelisib, though clinicians must monitor for hyperglycemia and rash.
CDK4/6 inhibitors themselves, when used as monotherapy or in combination with hormonal agents, arrest the cell‑cycle transition from G1 to S phase, thereby reducing tumor proliferation.
In the absence of a clear molecular target, standard chemotherapy or enrollment in clinical trials remains the mainstay of treatment.
Monitoring protocols are essential; HER2‑targeted agents require baseline and periodic cardiac echos, while CDK4/6 inhibitors demand regular complete blood counts to detect neutropenia.
Adverse effects differ among agents: HER2 therapies may cause cardiotoxicity, PI3K inhibitors can cause diarrhea, and PARP inhibitors often lead to photosensitivity.
Patients should maintain open communication with their oncology team to adjust doses promptly when side effects become intolerable.
Long‑term follow‑up with imaging every 2‑3 months helps assess response and detect early resistance, prompting a switch to alternative agents such as antibody‑drug conjugates or newer kinase inhibitors.
Emerging strategies include combination immunotherapy with CDK4/6 blockade, next‑generation HER2 antibody‑drug conjugates, and liquid biopsy‑guided dynamic treatment adjustments.
Overall, the key to success lies in a personalized, data‑driven approach that tailors therapy to the tumor’s unique molecular fingerprint while ensuring vigilant safety monitoring.
Mary Cautionary
One must appreciate the nuanced pharmacodynamics inherent to HER2‑directed monoclonal antibodies, as they exemplify the convergence of molecular oncology and bioengineered therapeutics.
Crystal Newgen
Just a reminder that regular monitoring makes all the difference in managing side effects.
Hannah Dawson
The hype around PARP inhibitors often ignores the modest response rates beyond BRCA‑mutated cohorts, which is a glaring omission in most patient brochures.
Julie Gray
It is worth noting that the pharmaceutical industry’s control over companion diagnostic approvals raises concerns about potential conflicts of interest that are seldom disclosed to the public.
Lisa Emilie Ness
Consistency in follow‑up imaging is key
Emily Wagner
In the grand schema of oncogenic signaling, we observe a cascade where PI3K inhibitors act as downstream modulators, essentially dampening the proliferative signal.
Mark French
I totally get how overwhelming this can feel, but trust me – the docs got your back, and the treatments are really effective when matched right.
Daylon Knight
So you want the cheap version? Sure, just skip the testing and hope for the best, why not.
Jason Layne
The whole narrative about personalized medicine is a smokescreen designed by big pharma to lock patients into endless subscription therapies. They claim precision while quietly shelving data that shows rapid resistance development. Every new 'target' is just a way to extend the profit pipeline. Regulatory bodies are in their pocket, approving drugs with tepid evidence. Wake up before you sign another contract.
Hannah Seo
If you’ve just gotten your genomic report, start by discussing the HER2 status with your oncologist – it can open doors to trastuzumab or newer ADCs.
Victoria Unikel
Honestly, this whole thing feels endless, but keep tracking your side effects, it helps.
Lindsey Crowe
Sure, another “miracle” drug – because the old ones weren’t enough.
Rama Hoetzlein
The so‑called ‘breakthroughs’ are just repackaged chemotherapies in a shiny bottle 😒 stop buying the hype 🙄
Lorena Garcia
I’ve heard some patients swear by combining CDK4/6 inhibitors with hormone therapy – anyone else seen good results?
Dietra Jones
its cool how the side effects are manageable if you keep up with the blood tests lol
Victoria Guldenstern
One could argue that the very notion of targeting a singular molecular pathway is a reductionist fallacy that ignores the tumor’s ecological complexity
Yet the clinical trials persist, driven by profit motives and the allure of precision
Patients are left to navigate a labyrinth of biomarkers, each promising hope but delivering uncertainty
In the end, the medical community must reconcile scientific ambition with ethical responsibility
Bill Bolmeier
Don’t let the jargon scare you – you’ve got a team behind you and a roadmap that can adapt as your tumor evolves. Keep the communication open and stay proactive!